Excretory system
The Nephron
Parts of a Nephron: Nephrons are the functional units of the
kidneys. Each nephron consists of two parts: a renal corpuscle (KOR- pus-sul tiny
body), where blood plasma is filtered, and a renal tubule into which the filtered
fluid passes. The two components of a renal corpuscle are the glomerulus
(capillary network) and the glomerular (Bowman’s) capsule, a double-walled
epithelial cup that surrounds the glomerular capillaries. Blood plasma is
filtered in the glomerular capsule, and then the filtered fluid passes into the
renal tubule, which has three main sections. In the order that fluid passes
through them, the renal tubule consists of a (1) proximal convoluted tubule,
(2) loop of Henle (nephron loop), and (3) distal convoluted tubule. Proximal
denotes the part of the tubule attached to the glomerular capsule, and distal
denotes the part that is further away. Convoluted means the tubule is tightly
coiled rather than straight. The renal corpuscle and both convoluted tubules
lie within the renal cortex; the loop of Henle extends into the renal medulla,
makes a hairpin turn, and then returns to the renal cortex. The distal
convoluted tubules of several nephrons empty into a single collecting duct.
Collecting ducts then unite and con- verge into several hundred large papillary
ducts, which drain into the minor calyces. The collecting ducts and papillary
ducts extend from the renal cortex through the renal medulla to the renal
pelvis. So one kidney has about 1 million nephrons, but a much smaller number
of collecting ducts and even fewer papillary ducts. In a nephron, the loop of
Henle connects the proximal and distal convoluted tubules. The first part of the
loop of Henle dips into the renal medulla, where it is called the descending
limb of the loop of Henle. It then makes that hairpin turn and returns to the
renal cortex as the ascending limb of the loop of Henle. About 80–85% of the
nephrons are cortical nephrons. Their renal corpuscles lie in the outer portion
of the renal cortex, and they have short loops of Henle that lie mainly in the
cortex and penetrate only into the outer region of the renal medulla. The short
loops of Henle receive their blood supply from per tubular capillaries that
arise from efferent arterioles. The other 15–20% of the nephrons is juxta-
medullary nephrons (juxta- near to). Their renal corpuscles lie deep in the
cortex, close to the medulla, and they have a long loop of Henle that extends
into the deepest region of the medulla (Figure 26.5b). Long loops of Henle
receive their blood supply from peritubular capillaries and from the vasa recta
that arise from efferent arterioles. In addition, the ascending limb of the
loop of Henle of juxtamedullary nephrons consists of two portions: a thin
ascending limb followed by a thick ascending limb. The lumen of the thin
ascending limb is the same as in other areas of the renal tubule; it is only
the epithelium that is thinner. Nephrons with long loops of Henle enable the
kidneys to excrete very dilute or very concentrated urine.
Histology of the Nephron and Collecting Duct
A single layer of epithelial cells forms the entire wall of the glomerular capsule, renal tubule, and ducts. However, each part has distinctive histological features that reflect its particular functions. We will discuss them in the order that fluid flows through them: glomerular capsule, renal tubule, and collecting duct.
GLOMERULAR CAPSULE The glomerular
(Bowman’s) capsule consists of visceral and parietal layers. The visceral layer
consists of modified simple squamous epithelial cells called podocytes (PO ¯
-do¯-c¯ıts; podo- foot; -cytes cells). The many foot like projections of these
cells (pedicels) wrap around the single layer of endothelial cells of the
glomerular capillaries and form the inner wall of the capsule. The parietal
layer of the glomerular capsule consists of simple squamous epithelium and
forms the outer wall of the capsule. Fluid filtered from the glomerular
capillaries enters the capsular (Bowman’s) space, the space between the two
layers of the glomerular capsule. Think of the glomerulus as a fist punched into
a limp balloon (the glomerular capsule) until the fist is covered by two layers
of balloon (visceral and parietal layers) with a space in between (the capsular
space).
RENAL TUBULE AND COLLECTING DUCT
illustrates the histology of the cells that form the renal tubule and collecting
duct. In the proximal convoluted tubule, the cells are simple cuboidal
epithelial cells with a prominent brush border of microvilli on their apical
surface (surface facing the lumen). These microvilli, like those of the small
intestine, increase the surface area for reabsorption and secretion. The
descending limb of the loop of Henle and the first part of the ascending limb of
the loop of Henle (the thin ascending limb) are composed of simple squamous
epithelium. (Recall that cortical or short-loop nephrons lack the thin
ascending limb.) The thick ascending limb of the loop of Henle is composed of
simple cuboidal to low columnar epithelium. In each nephron, the final part of
the ascending limb of the loop of Henle makes contact with the afferent
arteriole serving that renal corpuscle (Figure 26.6a). Because the columnar
tubule cells in this region are crowded together, they are known as the macula
densa (macula spot; densa dense).
Alongside the macula densa, the wall of the afferent arteriole (and sometimes
the efferent arteriole) contains modified smooth muscle fibers called
juxtaglomerular (JG) cells. Together with the macula densa, they constitute the
juxtaglomerular apparatus (JGA). As you will see later, the JGA helps regulate
blood pressure within the kidneys. The distal convoluted tubule (DCT) begins a
short distance past the macula densa. In the last part of the DCT and
continuing into the collecting ducts, two different types of cells are present.
Most are principal cells, which have receptors for both antidiuretic hormone (ADH)
and aldosterone, two hormones that regulate their functions. A smaller number
are intercalated cells, which play a role in the homeostasis of blood pH. The
collecting ducts drain into large papillary ducts, which are lined by simple
columnar epithelium. The number of nephrons is constant from birth. Any
increase in kidney size is due solely to the growth of individual nephrons. If
nephrons are injured or become diseased, new ones do not form. Signs of kidney
dysfunction usually do not become apparent until function declines to less than
25% of normal because the remaining functional nephrons adapt to handle a
larger-than- normal load. Surgical removal of one kidney, for example, stimulates
hypertrophy (enlargement) of the remaining kidney, which eventually is able to
filter blood at 80% of the rate of two normal kidneys.
OVERVIEW OF RENAL PHYSIOLOGY / formation of urine
To produce urine, nephrons and collecting ducts perform three basic processes—glomerular filtration, tubular reabsorption, and tubular secretion:
● Glomerular filtration. In the first step of urine production, water and most solutes in blood plasma move across the wall of glomerular capillaries into the glomerular capsule and then into the renal tubule.
● Tubular reabsorption. As filtered fluid flows along the renal tubule and through the collecting duct, tubule cells reabsorb about 99% of the filtered water and many useful solutes. The water and solutes return to the blood as it flows through the peritubular capillaries and vasa recta. Note that the term reabsorption refers to the return of substances to the blood- stream. The term absorption, by contrast, means entry of new substances into the body, as occurs in the gastrointestinal tract.
● Tubular secretion. As fluid flows along the renal tubule and through the collecting duct, the tubule and duct cells secrete other materials, such as wastes, drugs, and excess ions, into the fluid. Notice that tubular secretion removes a substance from the blood. In other instances of secretion—for instance, secretion of hormones—cells release substances into interstitial fluid and blood.
Solutes in the fluid that drains into
the renal pelvis remain in the urine and are excreted. The rate of urinary
excretion of any solute is equal to its rate of glomerular filtration, plus its
rate of secretion, minus its rate of reabsorption. By filtering, reabsorbing,
and secreting, nephrons help maintain homeostasis of the blood’s volume and
composition. The situation is somewhat analogous to a recycling center: Garbage
trucks dump refuse into an input hopper, where the smaller refuse passes onto a
conveyor belt (glomerular filtration of plasma). As the conveyor belt carries
the garbage along, workers remove useful items, such as aluminum cans,
plastics, and glass containers (reabsorption). Other workers place additional
garbage left at the center and larger items onto the conveyor belt (secretion).
At the end of the belt, all remaining garbage falls into a truck for transport
to the landfill (excretion of wastes in urine).
GLOMERULAR FILTRATION
The fluid that enters the capsular space is called the glomerular filtrate. The fraction of blood plasma in the afferent arterioles of the kidneys that becomes glomerular filtrate is the filtration fraction. Although a filtration fraction of 0.16–0.20 (16–20%) is typical, the value varies considerably in both health and disease. On average, the daily volume of glomerular filtrate in adults is 150 liters in females and 180 liters in males. More than 99% of the glomerular filtrate returns to the bloodstream via tubular reabsorption, so only 1–2 liters (about 1–2 qt) are excreted as urine.
The Filtration Membrane
Together, the endothelial cells of
glomerular capillaries and the podocytes, which completely encircle the
capillaries, form a leaky barrier known as the filtration membrane. This sandwich
like assembly permits filtration of water and small solutes but prevents
filtration of most plasma proteins, blood cells, and platelets. Substances
filtered from the blood cross three barriers—a glomerular endothelial cell, the
basal lamina, and a filtration slit formed by a podocytes
● Glomerular endothelial cells are quite leaky because they have large fenestrations (pores) that measure 0.07–0.1 m in diameter. This size permits all solutes in blood plasma to exit glomerular capillaries but prevents filtration of blood cells and platelets. Located among the glomerular capillaries and in the cleft between afferent and efferent arterioles are mesangial cells (mes- in the middle; -angi blood vessel). These contractile cells help regulate glomerular filtration.
● The basal lamina, a layer of
acellular material between the endothelium and the podocytes, consists of
minute collagen fibers and proteoglycans in a glycoprotein matrix; it pre- vents
filtration of larger plasma proteins.
● Extending from each podocyte are thousands of foot like processes termed pedicels (PED-i-sels little feet) that wrap around glomerular capillaries. The spaces between pedicels are the filtration slits. A thin membrane, the slit membrane, extends across each filtration slit; it permits the passage of molecules having a diameter smaller than 0.006–0.007 m, including water, glucose, vitamins, amino acids, very small plasma proteins, ammonia, urea, and ions. Less than 1% of albumin, the most plentiful plasma protein, passes the slit membrane because, with a diameter of 0.007m, it is slightly too big to get through.
The principle of filtration—the use of
pressure to force fluids and solutes through a membrane—is the same in
glomerular capillaries as in capillaries elsewhere in the body (see Starling’s
law of the capillaries, page 770). However, the volume of fluid filtered by the
renal corpuscle is much larger than in other capillaries of the body for three
reasons:
1. Glomerular capillaries present a large surface area for filtration because they are long and extensive. The mesangial cells regulate how much of this surface area is available for filtration. When mesangial cells are relaxed, surface area is maximal, and glomerular filtration is very high. Contraction of mesangial cells reduces the available surface area, and glomerular filtration decreases.
2. The filtration membrane is thin and porous.
Despite having several layers, the thickness of the filtration membrane is only
0.1 m. Glomerular capillaries also are about 50 times leakier than capillaries
in most other tissues, mainly because of their large fenestrations.
3. Glomerular capillary blood pressure is
high. Because the efferent arteriole is smaller in diameter than the afferent
arteriole, resistance to the outflow of blood from the glomerulus is high. As a
result, blood pressure in glomerular capillaries is considerably higher than in
capillaries elsewhere in the body.
Net Filtration Pressure
Glomerular filtration depends on three main pressures. One pressure promotes filtration and two pressures oppose filtration.
● Glomerular blood hydrostatic pressure (GBHP) is the blood pressure in glomerular capillaries. Generally, GBHP is about 55 mmHg. It promotes filtration by forcing water and solutes in blood plasma through the filtration membrane.
● Capsular hydrostatic pressure (CHP)
is the hydrostatic pressure exerted against the filtration membrane by fluid
already in the capsular space and renal tubule. CHP opposes filtration and
represents a “back pressure” of about 15 mmHg.
● Blood colloid osmotic pressure
(BCOP), which is due to the presence of proteins such as albumin, globulins,
and fibrinogen in blood plasma, also opposes filtration. The average BCOP in
glomerular capillaries is 30 mmHg.
Net filtration pressure (NFP), the
total pressure that promotes filtration, is determined as follows:
Net Filtration Pressure (NFP) + GBHP
- CHP -BCOP
By substituting the values just
given, normal NFP may be calculated:
NFP = 55 mmHg - 15 mmHg - 30 mmHg =10
mmHg
Thus, a pressure of only 10 mmHg
causes a normal amount of blood plasma (minus plasma proteins) to filter from
the glomerulus into the capsular space.
Glomerular Filtration Rate
The amount of filtrate formed in all
the renal corpuscles of both kidneys each minute is the glomerular filtration
rate (GFR). In adults, the GFR averages 125 mL/min in males and 105 mL/min in
females. Homeostasis of body fluids requires that the kidneys maintain a
relatively constant GFR. If the GFR is too high, needed substances may pass so
quickly through the renal tubules that some are not reabsorbed and are lost in
the urine. If the GFR is too low, nearly all the filtrate may be reabsorbed and
certain waste products may not be adequately excreted. GFR is directly related
to the pressures that determine net filtration pressure; any change in net
filtration pressure will affect GFR. Severe blood loss, for example, reduces
mean arterial blood pressure and decreases the glomerular blood hydrostatic
pressure. Filtration ceases if glomerular blood hydrostatic pressure drops to
45 mmHg because the opposing pressures add up to 45 mmHg. Amazingly, when
systemic blood pressure rises above normal, net filtration pressure and GFR
increase very little. GFR is nearly constant when the mean arterial blood
pressure is anywhere between 80 and 180 mmHg.
The mechanisms that regulate
glomerular filtration rate operate in two main ways:
(1) By adjusting blood flow into and out of the
glomerulus and
(2) By altering the glomerular capillary
surface area available for filtration. GFR increases when blood flow into the
glomerular capillaries increases. Coordinated control of the diameter of both
afferent and efferent arterioles regulates glomerular blood flow. Constriction
of the afferent arteriole decreases blood flow into the glomerulus; dilation of
the afferent arteriole increases it. Three mechanisms control GFR: renal auto regulation,
neural regulation, and hormonal regulation.
Renal Auto regulation of GFR the
kidneys themselves help maintain a constant renal blood flow and GFR despite
normal, everyday changes in blood pressure, like those that occur during
exercise. This capability is called renal auto regulation and consists of two
mechanisms— the myogenic mechanism and tubuloglomerular feedback. Working
together, they can maintain nearly constant GFR over a wide range of systemic blood
pressures. The myogenic mechanism (myo-
muscle; -genic producing) occurs
when stretching triggers contraction of smooth muscle cells in the walls of
afferent arterioles. As blood pressure rises, GFR also rises because renal
blood flow increases. However, the elevated blood pressure stretches the walls
of the afferent arterioles. In response, smooth muscle fibers in the wall of the
afferent arteriole contract, which narrows the arteriole’s lumen. As a result,
renal blood flow decreases, thus reducing GFR to its previous level. Conversely,
when arterial blood pressure drops, the smooth muscle cells are stretched less
and thus relax. The afferent arterioles dilate, renal blood flow increases, and
GFR increases. The myogenic mechanism normalizes renal blood flow and GFR within
seconds after a change in blood pressure. The second contributor to renal auto
regulation, tubuloglomerular feedback, is so named because part of the renal
tubules—the macula densa—provides feedback to the glomerulus. When GFR is above
normal due to elevated systemic blood pressure, filtered fluid flows more rapidly
along the renal tubules. As a result, the proximal convoluted tubule and loop
of Henle have less time to reabsorb Na Cl and
water. Macula densa cells are thought to detect the increased delivery of Na Cl
and water and to inhibit release of nitric oxide (NO) from cells in the
juxtaglomerular apparatus (JGA). Because NO causes vasodilation, afferent
arterioles constrict when the level of NO declines. As a result, less blood
flows into the glomerular capillaries and GFR decreases. When blood pressure
falls, causing GFR to be lower than normal, the opposite sequence of events
occurs, although to a lesser degree. Tubuloglomerular feedback operates more
slowly than the myogenic mechanism.
Neural Regulation of GFR
Like most blood vessels of the body, those of the kidneys are supplied by sympathetic ANS fibers that release norepinephrine. Norepinephrine causes vasoconstriction through the activation of α1 receptors, which are particularly plentiful in the smooth muscle fibers of afferent arterioles. At rest, sympathetic stimulation is moderately low, the afferent and efferent arterioles are dilated, and renal auto regulation of GFR prevails. With moderate sympathetic stimulation, both afferent and efferent arterioles constrict to the same degree. Blood flow into and out of the glomerulus is restricted to the same extent, which decreases GFR only slightly. With greater sympathetic stimulation, however, as occurs during exercise or hemorrhage, vasoconstriction of the afferent arterioles predominates. As a result, blood flow into glomerular capillaries is greatly decreased, and GFR drops.
This lowering of renal blood flow has
two consequences:
(1) It reduces urine output, which helps
conserve blood volume.
(2) It permits greater blood flow to other body
tissues.
Hormonal Regulation of GFR
Two hormones contribute to regulation of GFR. Angiotensin II reduces GFR; atrial natriuretic peptide (ANP) increases GFR. Angiotensin II is a very potent vasoconstrictor that narrows both afferent and efferent arterioles and reduces renal blood flow, thereby decreasing GFR. Cells in the atria of the heart secrete atrial natriuretic peptide (ANP). Stretching of the atria, as occurs when blood volume increases, stimulates secretion of ANP. By causing relaxation of the glomerular mesangial cells, ANP increases the capillary surface area available for filtration. Glomerular filtration rate rises as the surface area increases.
TUBULAR REABSORPTION AND TUBULAR
SECRETION
Principles of Tubular Reabsorption and Secretion
The volume of fluid entering the
proximal convoluted tubules in just half an hour is greater than the total
blood plasma volume because the normal rate of glomerular filtration is so high.
Obviously some of this fluid must be returned somehow to the bloodstream.
Reabsorption—the return of most of the filtered water and many of the filtered
solutes to the bloodstream—is the second basic function of the nephron and
collecting duct. Normally, about 99% of the filtered water is reabsorbed.
Epithelial cells all along the renal tubule and duct carry out reabsorption,
but proximal convoluted tubule cells make the largest contribution. Solutes
that are reabsorbed by both active and passive processes include glucose, amino
acids, urea, and ions such as Na (sodium), K (potassium), Ca2 (calcium), Cl
(chloride), HCO3 (bicarbonate), and HPO42 (phosphate). Once fluid passes through
the proximal convoluted tubule, cells located more distally fine-tune the
reabsorption processes to maintain homeostatic balances of water and selected
ions. Most small proteins and peptides that pass through the filter also are
reabsorbed, usually via pinocytosis. To appreciate the magnitude of tubular
reabsorption and compare the amounts of substances those are filtered,
reabsorbed, and excreted in urine. The third function of nephrons and
collecting ducts is tubular secretion, the transfer of materials from the blood
and tubule cells into tubular fluid. Secreted substances include hydrogen ions
(H) K, ammonium ions (NH4), creatinine, and certain drugs such as penicillin.
Tubular secretion has two important
outcomes:
(1) The secretion of H helps control blood pH.
(2) The secretion of other substances
helps eliminate them from the body. As a result of tubular secretion, certain
substances pass from blood into urine and may be detected by a urinalysis. It
is especially important to test athletes for the presence of
performance-enhancing drugs such as anabolic steroids, plasma expanders,
erythropoietin, hCG, hGH, and amphetamines. Urine tests can also be used to
detect the presence of alcohol or illegal drugs such as marijuana, cocaine, and
heroin.
Reabsorption Routes a substance being
reabsorbed from the fluid in the tubule lumen can take one of two routes before
entering a peritubular capillary: It can move between adjacent tubule cells or
through an individual tubule cell along the renal tubule, tight junctions
surround and join neighboring cells to one another, much like the plastic rings
that hold a six-pack of soda cans together. The apical membrane (the tops of
the soda cans) contacts the tubular fluid, and the basolateral membrane (the
bottoms and sides of the soda cans) contacts interstitial fluid at the base and
sides of the cell. The tight junctions do not completely seal off the
interstitial fluid from the fluid in the tubule lumen. Fluid can leak between the
cells in a passive process known as paracellular reabsorption (para- beside). In some parts of the renal tubule,
the paracellular route is thought to account for up to 50% of the reabsorption
of certain ions and the water that accompanies them via osmosis. In
transcellular reabsorption (trans- across), a substance passes from the fluid in
the tubular lumen through the apical membrane of a tubule cell, across the
cytosol, and out into interstitial fluid through the basolateral membrane.
Transport Mechanisms When renal cells
transport solutes out of or into tubular fluid, they move specific substances in
one direction only. Not surprisingly, different types of transport proteins are
present in the apical and basolateral membranes. The tight junctions form a
barrier that prevents mixing of proteins in the apical and basolateral membrane
compartments. Reabsorption of Na by the renal tubules is especially important
because of the large number of sodium ions that pass through the glomerular
filters. Cells lining the renal tubules, like other cells throughout the body,
have a low concentration of Na in their
cytosol due to the activity of sodium–potassium pumps (Na /K ATPases). These pumps are located in the basolateral
membranes and eject Na from the renal tubule cells. The absence of
sodium–potassium pumps in the apical membrane ensures that reabsorption of Na is
a one-way process. Most sodium ions that cross the apical membrane will be
pumped into interstitial fluid at the base and sides of the cell. The amount of
ATP used by sodium–potassium pumps in the renal tubules is about 6% of the
total ATP consumption of the body at rest. This may not sound like much, but it
is about the same amount of energy used by the diaphragm as it contracts during
quiet breathing. Transport of materials across membranes may be either active
or passive. Recall that in primary active transport the energy derived from
hydrolysis of ATP is used to “pump” a substance across a membrane; the sodium–
potassium pump is one such pump. In secondary active transport the energy
stored in an ion’s electrochemical gradient, rather than hydrolysis of ATP,
drives another substance across a membrane. Secondary active transport couples
the movement of an ion down its electrochemical gradient to the “uphill”
movement of a second substance against its electrochemical gradient. Symporters
are membrane proteins that move two or more substances in the same direction
across a membrane. Antiporters move two or more substances in opposite
directions across a membrane. Each type of transporter has an upper limit on
how fast it can work, just as an escalator has a limit on how many people it
can carry from one level to another in a given period. This limit, called the
transport maximum (Tm), is measured in mg/min. Solute reabsorption drives water
reabsorption because all water reabsorption occurs via osmosis. About 90% of
the reabsorption of water filtered by the kidneys occurs along with the reabsorption
of solutes such as Na, Cl and glucose. Water reabsorbed with solutes in
tubular fluid is termed obligatory water reabsorption (ob-LIG-a-tor-e¯) because
the water is “obliged” to follow the solutes when they are reabsorbed. This type
of water reabsorption occurs in the proximal convoluted tubule and the
descending limb of the loop of Henle because these segments of the nephron are
always permeable to water. Reabsorption of the final 10% of the water, a total
of 10–20 liters per day, is termed facultative water reabsorption
(FAK-ul-ta¯-tiv). The word facultative means “capable of adapting to a need.”
Facultative water reabsorption is regulated by antidiuretic hormone and occurs
mainly in the collecting ducts.
Now that we have discussed the
principles of renal transport, we will follow the filtered fluid from the
proximal convoluted tubule, into the loop of Henle, on to the distal convoluted
tubule, and through the collecting ducts. In each segment, we will ex- amine
where and how specific substances are reabsorbed and secreted. The filtered fluid
becomes tubular fluid once it enters the proximal convoluted tubule. The
composition of tubular fluid changes as it flows along the nephron tubule and
through the collecting duct due to reabsorption and secretion. The fluid that
drains from papillary ducts into the renal pelvis is urine.
Reabsorption and Secretion in the Proximal Convoluted Tubule
The largest amount of solute and water reabsorption from filtered fluid occurs in the proximal convoluted tubules, which reabsorb 65% of the filtered water, Na, and K; 100% of most filtered organic solutes such as glucose and amino acids; 50% of the filtered Cl; 80–90% of the filtered HCO3; 50% of the filtered urea; and a variable amount of the filtered Ca2, Mg 2, and HPO42 (phosphate). In addition, proximal convoluted tubules secrete a variable amount of H ions, ammonium ions (NH4), and urea. Most solute reabsorption in the proximal convoluted tubule (PCT) involves Na. Na transport occurs via symport and anti- port mechanisms in the proximal convoluted tubule. Normally, filtered glucose, amino acids, lactic acid, water-soluble vitamins, and other nutrients are not lost in the urine. Rather, they are completely reabsorbed in the first half of the proximal convoluted tubule by several types of Na symporters located in the apical membrane. Figure 26.12 depicts the operation of one such symporter, the Na–glucose symporter in the apical membrane of a cell in the PCT. Two Na and a molecule of glucose attach to the symporter protein, which carries them from the tubular fluid into the tubule cell. The glucose molecules then exit the basolateral membrane via facilitated diffusion and they diffuse into peritubular capillaries. Other Na symporters in the PCT reclaim filtered HPO42 (phosphate) and SO42 (sulfate) ions, all amino acids, and lactic acid in a similar way. In another secondary active transport process, the Na/H Antiporters carry filtered Na down its concentration gradient into a PCT cell as His moved from the cytosol into the lumen causing Na to be reabsorbed into blood and H to be secreted into tubular fluid. PCT cells produce the H needed to keep the antiporters running in the following way. Carbon dioxide (CO2) diffuses from peritubular blood or tubular fluid or is produced by metabolic reactions within the cells. As also occurs in red blood cells the enzyme carbonic anhydrase (CA) catalyzes the reaction of CO2 with water (H2O) to form carbonic acid (H2CO3), which then dissociates into H and HCO3:
CO2 + H2O ------> H
2CO3 ----------> H+
+ HCO3-
Most of the HCO3 in filtered fluid is reabsorbed
in proximal convoluted tubules, thereby safeguarding the body’s supply of an
important buffer. After H is secreted into the fluid within the lumen of the
proximal convoluted tubule, it re- acts with filtered HCO3 to form H2CO3, which
readily dissociates into CO2 and H2O. Carbon dioxide then diffuses into the
tubule cells and joins with H2O to form H2CO3, which dissociates into H and
HCO3. As the level of HCO3 rises in the cytosol, it exits via facilitated diffusion
transporters in the basolateral membrane and diffuses into the blood with Na.
Thus, for every H secreted into the tubular fluid of the proximal convoluted
tubule, one HCO3 and one Na are reabsorbed. Solute reabsorption in proximal
convoluted tubules promotes osmosis of water. Each reabsorbed solute increases
the osmolarity, first inside the tubule cell, then in interstitial fluid, and
finally in the blood. Water thus moves rapidly from the tubular fluid, via both
the paracellular and transcellular routes, into the peritubular capillaries and
restores osmotic balance. In other words reabsorption of the solutes creates an
osmotic gradient that promotes the reabsorption of water via osmosis. Cells
lining the proximal convoluted tubule and the descending limb of the loop of
Henle are especially permeable to water because they have many molecules of
aquaporin-1. This integral protein in the plasma membrane is a water channel
that greatly increases the rate of water movement across the apical and
basolateral membranes. As water leaves the tubular fluid, the concentrations of
the remaining filtered solutes increase. In the second half of the PCT,
electrochemical gradients for Cl, K , Ca 2, Mg 2, and urea promote their
passive diffusion into peritubular capillaries via both paracellular and
transcellular routes. Among these ions, Cl is present in the highest
concentration. Diffusion of negatively charged Cl into interstitial fluid via
the paracellular route makes the interstitial fluid electrically more negative
than the tubular fluid. This negativity promotes passive paracellular reabsorption
of cations, such as K, Ca 2, and Mg2. Ammonia (NH3) is a poisonous waste product
derived from the deamination (removal of an amino group) of various amino
acids, a reaction that occurs mainly in hepatocytes (liver cells). Hepatocytes
convert most of this ammonia to urea, a less-toxic compound. Although tiny
amounts of urea and ammonia are present in sweat, most excretion of these
nitrogen-containing waste products occurs via the urine. Urea and ammonia in
blood are both filtered at the glomerulus and secreted by proximal convoluted
tubule cells into the tubular fluid. Proximal convoluted tubule cells can
produce additional NH3 by deaminating the amino acid glutamine in a reaction
that also generates HCO3. The NH3 quickly binds H to become an ammonium ion
(NH4), which can substitute for H aboard Na /H antiporters in the apical
membrane and be secreted into the tubular fluid. The HCO3 generated in this
reaction moves through the basolateral membrane and then diffuses into the
bloodstream, providing additional buffers in blood plasma.
Reabsorption in the Loop of Henle
Because all of the proximal convoluted tubules reabsorb about 65% of the filtered water (about 80 mL/min), fluid enters the next part of the nephron, the loop of Henle, at a rate of 40–45 mL/min. The chemical composition of the tubular fluid now is quite different from that of glomerular filtrate because glucose, amino acids, and other nutrients are no longer present. The osmolarity of the tubular fluid is still close to the osmolarity of blood, however, because reabsorption of water by osmosis keeps pace with reabsorption of solutes all along the proximal convoluted tubule. The loop of Henle reabsorbs about 15% of the filtered water; 20–30% of the filtered Na and K; 35% of the filtered Cl; 10–20% of the filtered HCO3; and a variable amount of the filtered Ca2 and Mg2. Here, for the first time, reabsorption of water via osmosis is not automatically coupled to reabsorption of filtered solutes because part of the loop of Henle is relatively impermeable to water. The loop of Henle thus sets the stage for independent regulation of both the volume and osmolarity of body fluids.
The apical membranes of cells in the
thick ascending limb of the loop of Henle have Na–K–2Cl symporters that simultaneously
reclaim one Na, one K, and two Cl from the fluid in the tubular lumen. Na that
is actively trans- ported into interstitial fluid at the base and sides of the
cell diffuses into the vasa recta. Cl moves through leakage channels in the
basolateral membrane into interstitial fluid and then into the vasa recta.
Because many K leakage channels are present in the apical membrane, most K brought
in by the symporters moves down its concentration gradient back into the
tubular fluid. Thus, the main effect of the Na–K–2Cl symporters is reabsorption
of Na and Cl. The movement of positively charged K into the tubular fluid
through the apical membrane channels leaves the interstitial fluid and blood
with more negative charges relative to fluid in the ascending limb of the loop
of Henle. This relative negativity promotes reabsorption of cations—Na, K, Ca
2, and Mg2— via the paracellular route. Although about 15% of the filtered water
is reabsorbed in the descending limb of the loop of Henle, little or no water
is reabsorbed in the ascending limb. In this segment of the tubule, the apical
membranes are virtually impermeable to water. Because ions but not water
molecules are reabsorbed, the osmolarity of the tubular fluid decreases
progressively as fluid flows toward the end of the ascending limb.
Reabsorption in the Early Distal
Convoluted Tubule
Fluid enters the distal convoluted tubules
at a rate of about 25 mL/min because 80% of the filtered water has now been re-
absorbed. The early or initial part of the distal convoluted tubule (DCT)
reabsorbs about 10–15% of the filtered water; 5% of the filtered Na; and 5% of
the filtered Cl. Reabsorption of Na and
Cl occurs by means of Na–Cl symporters in the apical membranes.
Sodium–potassium pumps and Cl leakage channels in the basolateral membranes
then permit reabsorption of Na and Cl into the peritubular capillaries. The
early DCT also is a major site where parathyroid hormone (PTH) stimulates re-
absorption of Ca2. The amount of Ca2reabsorption in the early DCT varies
depending on the body’s needs.
Reabsorption and Secretion in the
Late Distal Convoluted Tubule and Collecting Duct
By the time fluid reaches the end of
the distal convoluted tubule, 90–95% of the filtered solutes and water have
returned to the bloodstream. Recall that two different types of cells—principal
cells and intercalated cells—are present at the late or terminal part of the
distal convoluted tubule and throughout the collecting duct. The principal
cells reabsorb Na and secrete K; the intercalated cells reabsorb K and HCO3 and
secrete H. In the late distal convoluted tubules and collecting ducts, the
amount of water and solute reabsorption and the amount of solute secretion vary
depending on the body’s needs.
In contrast to earlier segments of the
nephron, Na passes through the apical membrane of principal cells via Na leakage
channels rather than by means of symporters or antiporters. The concentration
of Na in the cytosol remains low, as usual, because the sodium–potassium pumps
actively transport Na across the basolateral membranes. Then Na passively
diffuses into the peritubular capillaries from the interstitial spaces around
the tubule cells. Normally, transcellular and paracellular reabsorption in the
proximal convoluted tubule and loop of Henle return most filtered K to the
bloodstream. To adjust for varying dietary intake of potassium and to maintain
a stable level of K in body fluids, principal cells secrete a variable amount of
K. Because the basolateral sodium–potassium pumps continually bring K into
principal cells, the intracellular concentration of K remains high. K leakage
channels are present in both the apical and basolateral membranes. Thus, some K
diffuses down its concentration gradient into the tubular fluid, where the K concentration
is very low. This secretion mechanism is the main source of K excreted in the
urine.
Hormonal Regulation of Tubular Reabsorption and Tubular Secretion/kidney hormones
Five hormones affect the extent of Na, Cl, Ca 2, and water reabsorption as well as K secretion by the renal tubules. These hormones include angiotensin II, aldosterone, antidiuretic hormone, atrial natriuretic peptide, and parathyroid hormone.
Renin–Angiotensin–Aldosterone System
When blood volume and blood pressure decrease, the walls of the afferent
arterioles are stretched less, and the juxtaglomerular cells secrete the enzyme
renin into the blood. Sympathetic stimulation also directly stimulates release
of renin from juxta- glomerular cells. Renin clips off a 10-amino-acid peptide
called angiotensin I from angiotensinogen, which is synthesized by hepatocytes.
By clipping off two more amino acids, angiotensin converting enzyme (ACE)
converts angiotensin I to angiotensin II, which is the active form of the
hormone. Angiotensin II affects renal physiology in three main ways:
1. It decreases the glomerular filtration
rate by causing vasoconstriction of the afferent arterioles.
2. It enhances reabsorption of Na, Cl, and
water in the proximal convoluted tubule by stimulating the activity of Na/H antiporters.
3. It stimulates the adrenal cortex to release
aldosterone, a hormone that in turn stimulates the principal cells in the
collecting ducts to reabsorb more Na and Cl and secrete more K. The osmotic
consequence of reabsorbing more Na and Cl is excreting less water, which
increases blood volume.
Antidiuretic Hormone Antidiuretic
hormone (ADH or vasopressin) is released by the posterior pituitary. It
regulates facultative water reabsorption by increasing the water permeability
of principal cells in the last part of the distal convoluted tubule and
throughout the collecting duct. In the absence of ADH, the apical membranes of
principal cells have a very low permeability to water. Within principal cells
are tiny vesicles containing many copies of a water channel protein known as
aquaporin-2.* ADH stimulates insertion of the aquaporin-2–containing vesicles
into the apical membranes via exocytosis. As a result, the water permeability
of the principal cell’s apical membrane increases, and water molecules move
more rapidly from the tubular fluid into the cells. Because the basolateral
membranes are always relatively permeable to water, water molecules then move
rapidly into the blood. The kidneys can produce as little as 400–500 mL of very
concentrated urine each day when ADH concentration is maximal, for instance
during severe dehydration. When ADH level declines, the aquaporin-2 channels
are removed from the apical membrane via endocytosis. The kidneys produce a
large volume of dilute urine when ADH level is low. A negative feedback system
involving ADH regulates facultative water reabsorption. When the osmolarity or
osmotic pressure of plasma and interstitial fluid increases—that is, when water
concentration decreases—by as little as 1%, osmo receptors in the hypothalamus
detect the change. Their nerve impulses stimulate secretion of more ADH into
the blood, and the principal cells become more permeable to water. As facultative
water reabsorption increases, plasma osmolarity decreases to normal. A second
powerful stimulus for ADH secretion is a decrease in blood volume, as occurs in
hemorrhaging or severe dehydration. In the pathological absence of ADH
activity, a condition known as diabetes insipidus, a person may excrete up to
20 liters of very dilute urine daily.
Atrial Natriuretic Peptide a large
increase in blood volume promotes release of atrial natriuretic peptide (ANP)
from the heart. Although the importance of ANP in normal regulation of tubular
function is unclear, it can inhibit reabsorption of Na and water in the
proximal convoluted tubule and collecting duct. ANP also suppresses the secretion
of aldosterone and ADH. These effects increase the excretion of Na in urine
(natriuresis) and increase urine output (diuresis), which decreases blood
volume and blood pressure.
Parathyroid Hormone A
lower-than-normal level of Ca2 in the blood stimulates the parathyroid glands
to release parathyroid hormone (PTH). PTH in turn stimulates cells in the early
distal convoluted tubules to reabsorb more Ca2 into the blood. PTH also
inhibits HPO42 (phosphate) reabsorption in proximal convoluted tubules, thereby
promoting phosphate excretion. Table 26.4 summarizes hormonal regulation of
tubular reabsorption and tubular secretion.
PRODUCTION OF DILUTE AND CONCENTRATED URINE
OBJECTIVE
• Describe how the renal tubule and collecting
ducts pro- duce dilute and concentrated urine.
Even though your fluid intake can be
highly variable, the total volume of fluid in your body normally remains stable.
Homeostasis of body fluid volume depends in large part on the ability of the
kidneys to regulate the rate of water loss in urine. Normally functioning
kidneys produce a large volume of dilute urine when fluid intake is high, and a small volume of concentrated urine
when fluid intake is low or fluid loss is large. ADH controls whether dilute
urine or concentrated urine is formed. In the absence of ADH, urine is very
dilute. However, a high level of ADH stimulates reabsorption of more water into
blood, producing concentrated urine.
Formation of Dilute Urine
Glomerular filtrate has the same ratio of water and solute particles as blood; its osmolarity is about 300mOsm/liter. As previously noted, fluid leaving the proximal convoluted tubule is still isotonic to plasma. When dilute urine is being formed, the osmolarity of the fluid in the tubular lumen increases as it flows down the descending limb of the loop of Henle, decreases as it flows up the ascending limb, and decreases still more as it flows through the rest of the nephron and collecting duct. These changes in osmolarity result from the following conditions along the path of tubular fluid:
1.
Because
the osmolarity of the interstitial fluid of the renal medulla becomes
progressively greater, more and more water is reabsorbed by osmosis as tubular
fluid flows along the descending limb toward the tip of the loop. (The source of
this medullary osmotic gradient is explained shortly.) As a result, the fluid
remaining in the lumen becomes progressively more concentrated.
2.
Cells lining the thick ascending limb of the
loop have symporters that actively reabsorb Na, K, and Cl from the tubular fluid. The ions pass from the
tubular fluid into thick ascending limb cells, then into interstitial fluid, and
finally some diffuse into the blood inside the vasa recta.
3.
Although solutes are being reabsorbed in the
thick ascending limb, the water permeability of this portion of the nephron is
always quite low, so water cannot follow by osmosis. As solutes—but not water
molecules—are leaving the tubular fluid, its osmolarity drops to about 150
mOsm/liter. The fluid entering the distal convoluted tubule is thus more dilute
than plasma.
4.
While the fluid continues flowing along the
distal convoluted tubule, additional solutes but only a few water molecule are
reabsorbed. The early distal convoluted tubule cells are not very permeable to
water and are not regulated by ADH.
5.
Finally,
the principal cells of the late distal convoluted tubules and collecting ducts
are impermeable to water when the ADH level is very low. Thus, tubular fluid
becomes progressively more dilute as it flows onward. By the time the tubular
fluid drains into the renal pelvis, its concentration can be as low as 65–70
mOsm/liter. This is four times more dilute than blood plasma or glomerular
filtrate.
Formation of Concentrated Urine
When water intake is low or water loss is high (such as during heavy sweating), the kidneys must conserve water while still eliminating wastes and excess ions. Under the influence of ADH, the kidneys produce a small volume of highly concentrated urine. Urine can be four times more concentrated (up to 1200 mOsm/liter) than blood plasma or glomerular filtrate (300mOsm/liter). The ability of ADH to cause excretion of concentrated urine depends on the presence of an osmotic gradient of solutes in the interstitial fluid of the renal medulla. The solute concentration of the interstitial fluid in the kidney increases from about 300 mOsm/liter in the renal cortex to about 1200 mOsm/liter deep in the renal medulla. The three major solutes that contribute to this high osmolarity are Na, Cl, and urea. Two main factors contribute to building and maintaining this osmotic gradient:
When water intake is low or water loss is high (such as during heavy sweating), the kidneys must conserve water while still eliminating wastes and excess ions. Under the influence of ADH, the kidneys produce a small volume of highly concentrated urine. Urine can be four times more concentrated (up to 1200 mOsm/liter) than blood plasma or glomerular filtrate (300mOsm/liter). The ability of ADH to cause excretion of concentrated urine depends on the presence of an osmotic gradient of solutes in the interstitial fluid of the renal medulla. The solute concentration of the interstitial fluid in the kidney increases from about 300 mOsm/liter in the renal cortex to about 1200 mOsm/liter deep in the renal medulla. The three major solutes that contribute to this high osmolarity are Na, Cl, and urea. Two main factors contribute to building and maintaining this osmotic gradient:
(1) Differences in solute and water
permeability and reabsorption in different sections of the long loops of Henle
and the collecting ducts
(2) The countercurrent flow of fluid through tube-shaped
structures in the renal medulla. Countercurrent flow refers to the flow of fluid
in opposite directions. This occurs when fluid flowing in one tube runs counter
(opposite) to fluid flowing in a nearby parallel tube.
Examples of countercurrent flow include the flow
of tubular fluid through the descending and ascending limbs of the loop of Henle
and the flow of blood through the ascending and descending parts of the vasa
recta. Two types of countercurrent mechanisms exist in the kidneys:
countercurrent multiplication and countercurrent exchange.
Countercurrent Multiplication
Countercurrent multiplication is the process
by which a progressively increasing osmotic gradient is formed in the interstitial
fluid of the renal medulla as a result of countercurrent flow. Countercurrent
multiplication involves the long loops of Henle of juxtamedullary nephrons. the
descending limb of the loop of Henle carries tubular fluid from the renal cortex
deep into the medulla, and the ascending limb carries it in the opposite
direction. Since countercurrent flow through the descending and ascending limbs
of the long loop of Henle establishes the osmotic gradient in the renal
medulla, the long loop of Henle is said to function as a countercurrent multiplier.
The kidneys use this osmotic gradient to excrete concentrated urine. Production
of concentrated urine by the kidneys occurs in the following way.
Ø Symporters in thick ascending limb
cells of the loop of Henle cause a buildup of Na and Cl in the renal medulla.
In the thick ascending limb of the loop of Henle, the Na K 2Cl symporters
reabsorb Na and Cl from the tubular fluid. Water is not reabsorbed in this
segment, however, because the cells are impermeable to water. As a result,
there is a buildup of Na and Cl ions in the interstitial fluid of the medulla.
Ø Countercurrent flow through the
descending and ascending limbs of the loop of Henle establishes an osmotic gradient
in the renal medulla. Since tubular fluid constantly moves from the descending
limb to the thick ascending limb of the loop of Henle, the thick ascending limb
is constantly reabsorbing Na and Cl Consequently, the reabsorbed Na and Cl become
increasingly concentrated in the interstitial fluid of the medulla, which results
in the formation of an osmotic gradient that ranges from 300 mOsm/liter in the
outer medulla to 1200 mOsm/liter deep in the inner medulla. The descending limb
of the loop of Henle is very permeable to water but impermeable to solutes
except urea. Because the osmolarity of the interstitial fluid outside the
descending limb is higher than the tubular fluid within it, water moves out of
the descending limb via osmosis. This causes the osmolarity of the tubular fluid
to increase. As the fluid continues along the descending limb, its osmolarity
increases even more: At the hairpin turn of the loop, the osmolarity can be as
high as 1200 mOsm/liter in juxtamedullary nephrons. As you have already
learned, the ascending limb of the loop is impermeable to water, but its
symporters reabsorb Na and Cl from the tubular fluid into the interstitial
fluid of the renal medulla, so the osmolarity of the tubular fluid progressively
decreases as it flows through the ascending limb. At the junction of the medulla
and cortex, the osmolarity of the tubular fluid has fallen to about 100
mOsm/liter. Overall, tubular fluid becomes progressively more concentrated as it
flows along the descending limb and progressively more di- lute as it moves
along the ascending limb.
Ø Cells in the collecting ducts
reabsorb more water and urea. When ADH increases the water permeability of the
principal cells, water quickly moves via osmosis out of the collecting duct
tubular fluid, into the interstitial fluid of the inner medulla, and then into
the vasa recta. With loss of water, the urea left behind in the tubular fluid of
the collecting duct becomes increasingly concentrated. Because duct cells deep
in the medulla are permeable to it, urea diffuses from the fluid in the duct
into the interstitial fluid of the medulla.
Ø
Urea
recycling causes a buildup of urea in the renal medulla. As urea accumulates in
the interstitial fluid, some of it diffuses into the tubular fluid in the
descending and thin ascending limbs of the long loops of Henle, which also are
permeable to urea. However, while the fluid flows through the thick ascending
limb, distal convoluted tubule, and cortical portion of the collecting duct,
urea remains in the lumen because cells in these segments are impermeable to
it. As fluid flows along the collecting ducts, water reabsorption continues via
osmosis because ADH is present. This water reabsorption further increases the
con- centration of urea in the tubular fluid, more urea diffuses into the
interstitial fluid of the inner renal medulla, and the cycle repeats. The
constant transfer of urea between segments of the renal tubule and the
interstitial fluid of the medulla is termed urea recycling. In this way,
reabsorption of water from the tubular fluid of the ducts promotes the buildup
of urea in the interstitial fluid of the renal medulla, which in turn promotes
water reabsorption. The solutes left behind in the lumen thus become very
concentrated, and a small volume of concentrated urine is excreted.
Countercurrent Exchange
Countercurrent exchange is the process by which solutes and water are passively exchanged between the blood of the vasa recta and interstitial fluid of the renal medulla as a result of countercurrent flow. the vasa recta also consists of descending and ascending limbs that are parallel to each other and to the loop of Henle. Just as tubular fluid flows in opposite directions in the loop of Henle, blood flows in opposite directions in the ascending and descending parts of the vasa recta. Since countercurrent flow between the descending and ascending limbs of the vasa recta allows for exchange of solutes and water between the blood and interstitial fluid of the renal medulla, the vasa recta is said to function as a countercurrent exchanger. Blood entering the vasa recta has an osmolarity of about 300 mOsm/liter. As it flows along the descending part into the renal medulla, where the interstitial fluid becomes increasingly concentrated, Na, Cl, and urea diffuse from interstitial fluid into the blood and water diffuses from the blood into the interstitial fluid. But after its osmolarity increases, the blood flows into the ascending part of the vasa recta. Here blood flows through a region where the interstitial fluid becomes increasingly less concentrated. As a result Na, Cl, and urea diffuse from the blood back into interstitial fluid, and water diffuses from interstitial fluid back into the vasa recta. The osmolarity of blood leaving the vasa recta is only slightly higher than the osmolarity of blood entering the vasa recta. Thus, the vasa recta provide oxygen and nutrients to the renal medulla without washing out or diminishing the osmotic gradient. The long loop of Henle establishes the osmotic gradient in the renal medulla by countercurrent multiplication, but the vasa recta maintain the osmotic gradient in the renal medulla by countercurrent exchange.
EVALUATION OF KIDNEY
FUNCTION
Routine
assessment of kidney function involves evaluating both the quantity and quality
of urine and the levels of wastes in the blood.
Urinalysis
An analysis of
the volume and physical, chemical, and microscopic properties of urine, called
a urinalysis, reveals much about the state of the body. summarizes the
major characteristics of normal urine. The volume of urine eliminated per day
in a normal adult is 1–2 liters (about 1–2 qt). Fluid intake, blood pressure,
blood osmolarity, diet, body temperature, diuretics, mental state, and general
health influence urine volume. For example, low blood pressure triggers the
renin– angiotensin–aldosterone pathway. Aldosterone increases reabsorption of
water and salts in the renal tubules and decreases urine volume. By contrast,
when blood osmolarity decreases— for example, after drinking a large volume of
water—secretion of ADH is inhibited and a larger volume of urine is excreted.
Water accounts for about 95% of the total volume of urine. The remaining 5%
consists of electrolytes, solutes derived from cellular metabolism, and
exogenous substances such as drugs. Normal urine is virtually protein-free.
Typical solutes normally present in urine include filtered and secreted
electrolytes that are not reabsorbed, urea (from breakdown of proteins),
creatinine (from breakdown of creatine phosphate in muscle fibers), uric acid
(from breakdown of nucleic acids), urobilinogen (from breakdown of hemoglobin),
and small quantities of other sub- stances, such as fatty acids, pigments,
enzymes, and hormones. If disease alters body metabolism or kidney function,
traces of substances not normally present may appear in the urine, or normal
constituents may appear in abnormal amounts. Several abnormal constituents in
urine that may be detected as part of a urinalysis. Normal values of urine components
and the clinical implications of deviations from normal are listed in Appendix
D.
Blood Tests
Renal Plasma Clearance
Even more
useful than BUN and blood creatinine values in the diagnosis of kidney problems
is an evaluation of how effectively the kidneys are removing a given substance
from blood plasma. Renal plasma clearance is the volume of blood that is
“cleaned” or cleared of a substance per unit of time, usually expressed in
units of milliliters per minute. High renal plasma clearance indicates efficient
excretion of a substance in the urine; low clearance indicates inefficient
excretion. For example, the clearance of glucose normally is zero because it is
completely reabsorbed; therefore, glucose is not excreted at all. Knowing a
drug’s clearance is essential for deter- mining the correct dosage. If
clearance is high (one example is penicillin), then the dosage must also be
high, and the drug must be given several times a day to maintain an adequate
therapeutic level in the blood. The following equation is used to calculate
clearance:
Renal plasma
clearance of substance S = ((U X V)/p)
Where U and P
are the concentrations of the substance in urine and plasma, respectively (both
expressed in the same units, such as mg/mL), and V is the urine flow rate in
mL/min. The clearance of a solute depends on the three basic processes of a
nephron: glomerular filtration, tubular reabsorption, and tubular secretion.
Consider a substance that is filtered but neither reabsorbed nor secreted. Its
clearance equals the glomerular filtration rate because all the molecules that
pass the filtration membrane appear in the urine. This is very nearly the
situation for creatinine; it easily passes the filter, it is not reabsorbed, and
it is secreted only to a very small extent. Measuring the creatinine clearance,
which normally is 120– 140 mL/min, is the easiest way to assess glomerular
filtration rate. The waste product urea is filtered, reabsorbed, and secreted to
varying extents. Its clearance typically is less than the GFR, about 70 mL/min.
The clearance of the organic anion para-aminohippuric acid (PAH) is also of
clinical importance. After PAH is administered intravenously, it is filtered and
secreted in a single pass through the kidneys. Thus, the clearance of PAH is
used to measure renal plasma flow, the amount of plasma that passes through the
kidneys in one minute. Typically, the renal plasma flow is 650 mL per minute,
which is about 55% of the renal blood flow (1200 mL per minute).
Dialysis
If a person’s
kidneys are so impaired by disease or injury that he or she is unable to
function adequately, then blood must be cleansed artificially by dialysis
(d¯ı-AL-i-sis; dialyo to separate), the
separation of large solutes from smaller ones by diffusion through a
selectively permeable membrane. One method of dialysis is hemodialysis
(he¯-mo¯-d¯ı- AL-i-sis; hemo- blood),
which directly filters the patient’s blood by re- moving wastes and excess
electrolytes and fluid and then returning the cleansed blood to the patient.
Blood removed from the body is delivered to a hemodialyzer (artificial kidney).
Inside the hemodialyzer, blood flows through a dialysis membrane, which contains
pores large enough to permit the diffusion of small solutes. A special solution,
called the dialysate (dı¯-AL-i-sa¯t), is pumped into the hemodialyzer so that
it surrounds the dialysis membrane. The dialysate is especially formulated to
maintain diffusion gradients that remove wastes from the blood (for example,
urea, creatinine, uric acid, excess phosphate, potassium, and sulfate ions) and
add needed substances (for example, glucose and bicarbonate ions) to it. The
cleansed blood is passed through an air embolus detector to remove air and then
returned to the body. An anticoagulant (heparin) is added to prevent blood from
clot- ting in the hemodialyzer. As a rule, most people on hemodialysis require
about 6–12 hours a week, typically divided into three sessions. Another method
of dialysis, called peritoneal dialysis, uses the peritoneum of the abdominal
cavity as the dialysis membrane to filter the blood. The peritoneum has a large
surface area and numerous blood vessels, and is a very effective filter. A
catheter is inserted into the peritoneal cavity and connected to a bag of
dialysate. The fluid flows into the peritoneal cavity by gravity and is left
there for sufficient time to permit wastes and excess electrolytes and fluids to
diffuse into the dialysate. Then the dialysate is drained out into a bag,
discarded, and replaced with fresh dialysate. Each cycle is called an exchange.
One variation of peritoneal dialysis, called continuous ambulatory peritoneal
dialysis (CAPD), can be per- formed at home. Usually, the dialysate is drained
and replenished four times a day and once at night during sleep. Between
exchanges the person can move about freely with the dialysate in the peritoneal
cavity.
Regulation of acid
base, electrolyte and water balance
In lean
adults, body fluids constitute between 55% and 60% of total body mass in females
and males, respectively. Body fluids are present in two main “compartments”—inside
cells and outside cells. About two-thirds of body fluid is intracellular fluid
(ICF) (intra- within) or cytosol, the
fluid within cells. The other third, called extracellular fluid (ECF)
(extra- outside) is outside cells and
includes all other body fluids. About 80% of the ECF is interstitial fluid
(inter- between), which occupies the microscopic spaces between tissue cells,
and 20% of the ECF is plasma, the liquid portion of the blood. Other
extracellular fluids that are grouped with interstitial fluid include lymph in
lymphatic vessels; cerebrospinal fluid in the nervous system; synovial fluid
in joints;
aqueous humor and vitreous body in the eyes; endolymph and perilymph in the
ears; and pleural, pericardial, and peritoneal fluids between serous membranes.
Two general “barriers” separate intracellular fluid, interstitial fluid, and
blood plasma.
1. The plasma
membrane of individual cells separates intra- cellular fluid from the
surrounding interstitial fluid. the plasma membrane is a selectively permeable
barrier: It allows some substances to cross but blocks the movement of other
substances. In addition, active transport pumps work continuously to maintain
different concentrations of certain ions in the cytosol and interstitial fluid.
2. Blood
vessel walls divide the interstitial fluid from blood plasma. Only in
capillaries, the smallest blood vessels, are the walls thin enough and leaky
enough to permit the exchange of water and solutes between blood plasma and
interstitial fluid.
The body is in
fluid balance when the required amounts of water and solutes are present and are
correctly proportioned among the various compartments. Water is by far the
largest single component of the body, making up 45–75% of total body mass,
depending on age and gender.
The processes
of filtration, reabsorption, diffusion, and osmosis allow continual exchange of
water and solutes among body fluid compartments. Yet the volume of fluid in each
compartment remains remarkably stable. The pressures that promote filtration of
fluid from blood capillaries and reabsorption of fluid back into capillaries can
be reviewed. Because osmosis is the primary means of water movement between
intracellular fluid and interstitial fluid, the concentration of solutes in these
fluids determines the direction of water movement. Because most solutes in body
flu- ids are electrolytes, inorganic compounds that dissociate into ions, fluid
balance is closely related to electrolyte balance. Because intake of water and electrolytes
rarely occurs in exactly the same proportions as their presence in body fluids,
the ability of the kidneys to excrete excess water by producing dilute urine,
or to excrete excess electrolytes by producing concentrated urine, is of utmost
importance in the maintenance of homeostasis.
Sources of Body Water
Gain and Loss
The body can
gain water by ingestion and by metabolic synthesis. The main sources of body
water are ingested liquids (about 1600 mL) and moist foods (about 700 mL) absorbed
from the gastrointestinal (GI) tract, which total about 2300 mL/day. The other
source of water is metabolic water that is produced in the body mainly when
electrons are accepted by oxygen during aerobic cellular respiration and to a
smaller extent during dehydration synthesis reactions. Metabolic water gain accounts
for only 200 mL/day. Daily water gain from these two sources totals about 2500mL.
Normally, body fluid volume remains constant because water loss equals water
gain. Water loss occurs in four ways. Each day the kidneys excrete about 1500
mL in urine, the skin evaporates about 600 mL (400 mL through insensible
perspiration, sweat that evaporates before it is perceived as moisture, and 200
mL as sweat), the lungs exhale about 300 mL as water vapor, and the
gastrointestinal tract eliminates about 100 mL in feces. In women of
reproductive age, additional water is lost in menstrual flow. On average, daily
water loss totals about 2500mL. The amount of water lost by a given route can
vary considerably over time. For example, water may literally pour from the
skin in the form of sweat during strenuous exertion. In other cases, water may
be lost in diarrhea during a GI tract infection.
Regulation of Body
Water Gain
The volume of
metabolic water formed in the body depends entirely on the level of aerobic
cellular respiration, which reflects the demand for ATP in body cells. When more
ATP is produced, more water is formed. Body water gain is regulated mainly by
the volume of water intake, or how much fluid you drink. An area in the
hypothalamus known as the thirst center governs the urge to drink. When water
loss is greater than water gain, dehydration— a decrease in volume and an
increase in osmolarity of body fluids—stimulates thirst. When body mass
decreases by 2% due to fluid loss, mild dehydration exists. A decrease in blood
volume causes blood pressure to fall. This change stimulates the kidneys to
release renin, which promotes the formation of angiotensin II. Increased nerve
impulses from osmo receptors in the hypothalamus, triggered by increased blood
osmolarity, and increased angiotensin II in the blood both stimulate the thirst
center in the hypothalamus. Other signals that stimulate thirst come from (1)
neurons in the mouth that detect dryness due to a decreased flow of saliva and
(2) baroreceptors that detect lowered blood pressure in the heart and blood
vessels. As a result, the sensation of thirst increases, which usually leads to
increased fluid intake (if fluids are available) and restoration of normal fluid
volume. Overall, fluid gain balances fluid loss. Sometimes, however, the
sensation of thirst does not occur quickly enough or access to fluids is
restricted, and significant dehydration ensues. This happens most often in
elderly people, in infants, and in those who are in a confused mental state.
When heavy sweating or fluid loss from diarrhea or vomiting occurs, it is wise
to start replacing body fluids by drinking fluids even before the sensation of
thirst occurs.
Regulation of Water and
Solute Loss
Even though
the loss of water and solutes through sweating and exhalation increases during
exercise, elimination of excess body water or solutes occurs mainly by control
of their loss in urine. The extent of urinary salt (NaCl) loss is the main
factor that determines body fluid volume. The reason for this is that “water
follows solutes” in osmosis, and the two main solutes in extra cellular fluid
(and in urine) are sodium ions (Na) and chloride ions (Cl). In a similar way,
the main factor that determines body fluid osmolarity is the extent of urinary
water loss. Because our daily diet contains a highly variable amount of NaCl,
urinary excretion of Na and Cl must also
vary to maintain homeostasis. Hormonal changes regulate the urinary loss of
these ions, which in turn affects blood volume. The sequence of changes that
occur after a salty meal. The increased intake of NaCl produces an increase in
plasma levels of Na and Cl (the major contributors to osmolarity of
extracellular fluid). As a result, the osmolarity of interstitial fluid
increases, which causes movement of water from intracellular fluid into
interstitial fluid and then into plasma. Such water movement increases blood
volume. The three most important hormones that regulate the extent of renal Na and
Cl reabsorption (and thus how much is lost in the urine) are angiotensin II,
aldosterone, and atrial natriuretic peptide (ANP). When your body is
dehydrated, angiotensin II and aldosterone promote urinary reabsorption of Na and
Cl (and water by osmosis with the electrolytes), conserving the volume of body
fluids by reducing urinary loss. An increase in blood volume, as might occur
after you finish one or more supersized drinks, stretches the atria of the heart
and promotes release of atrial natriuretic peptide. ANP promotes natriuresis,
elevated urinary excretion of Na (and Cl) followed by water excretion, which
decreases blood volume. An increase in blood volume also slows release of renin
from juxtaglomerular cells of the kidneys. When renin level declines, less
angiotensin II is formed. Decline in angiotensin II from a moderate level to a
low level increases glomerular filtration rate and reduces Na, Cl, and water
reabsorption in the kidney tubules. In addition, less angiotensin II leads to
lower levels of aldosterone, which causes reabsorption of filtered Na and Cl to
slow in the renal collecting ducts. More filtered Na and Cl thus remain in the
tubular fluid to be excreted in the urine. The osmotic consequence of excreting
more Na and Cl is loss of more water in urine, which decreases blood volume and
blood pressure. The major hormone that regulates water loss is antidiuretic
hormone (ADH). This hormone, also known as vasopressin, is produced by
neurosecretory cells that extend from the hypothalamus to the posterior
pituitary. In addition to stimulating the thirst mechanism, an increase in the
osmolarity of body fluids stimulates release of ADH. ADH promotes the insertion
of water-channel proteins (aquaporin-2) into the apical membranes of principal
cells in the collecting ducts of the kidneys. As a result, the permeability of
these cells to water increases. Water molecules move by osmosis from the renal
tubular fluid into the cells and then from the cells into the bloodstream. The
result is production of a small volume of very concentrated urine. Intake of
water in response to the thirst mechanism decreases the osmolarity of blood and
interstitial fluid. Within minutes, ADH secretion shuts down, and soon its blood
level is close to zero. When the principal cells are not stimulated by ADH,
aquaporin-2 molecules are removed from the apical membrane by endocytosis. As
the number of water channels decreases, the water permeability of the principal
cells’ apical membrane falls, and more water is lost in the urine. Under some
conditions, factors other than blood osmolarity influence ADH secretion. A large
decrease in blood volume, which is detected by baroreceptors (sensory neurons
that respond to stretching) in the left atrium and in blood vessel walls, also
stimulates ADH release. In severe dehydration, glomerular filtration rate
decreases because blood pressure falls, so that less water is lost in the
urine. Conversely, the intake of too much water increases blood pressure,
causing the rate of glomerular filtration to rise, and more water to be lost in
the urine. Hyperventilation (abnormally fast and deep breathing) can increase
fluid loss through the exhalation of more water vapor. Vomiting and diarrhea
result in fluid loss from the GI tract. Finally, fever, heavy sweating, and
destruction of extensive areas of the skin from burns can cause excessive water
loss through the skin. In all of these conditions, an increase in ADH secretion
will help conserve body fluids.
Movement of
Water between Body Fluid Compartments
Normally,
cells neither shrink nor swell because intracellular and interstitial fluids
have the same osmolarity. Changes in the osmolarity of interstitial fluid,
however, cause fluid imbalances. An increase in the osmolarity of interstitial
fluid draws water out of cells, and they shrink slightly. A decrease in the
osmolarity of interstitial fluid, by contrast, causes cells to swell. Changes in
osmolarity most often result from changes in the concentration of Na. A decrease in the osmolarity of interstitial
fluid, as may occur after drinking a large volume of water, inhibits secretion
of ADH. Normally, the kidneys then excrete a large volume of di- lute urine,
which restores the osmotic pressure of body fluids to normal. As a result, body
cells swell only slightly, and only for a brief period. But when a person
steadily consumes water faster than the kidneys can excrete it (the maximum
urine flow rate is about 15 mL/min) or when renal function is poor, the result
may be water intoxication, a state in which excessive body water causes cells
to swell dangerously. If the body water and Na lost during blood loss or
excessive sweating, vomiting, or diarrhea is replaced by drinking plain water,
then body fluids become more dilute. This dilution can cause the Na concentration
of plasma and then of interstitial fluid to fall below the normal range. When
the Na concentration of interstitial fluid decreases, its osmolarity also falls.
The net result is osmosis of water from interstitial fluid into the cytosol.
Water entering the cells causes them to swell, producing convulsions, coma, and
possibly death. To prevent this dire sequence of events in cases of severe
electrolyte and water loss, solutions given for intra- venous or oral
rehydration therapy (ORT) include a small amount of table salt (NaCl).
ELECTROLYTES IN BODY
FLUIDS
The ions
formed when electrolytes dissolve and dissociate serve four general functions
in the body.
(1) Because
they are largely confined to particular fluid compartments and are more numerous
than nonelectrolytes, certain ions control the osmosis of water between fluid
compartments.
(2) Ions help
maintain the acid–base balance required for normal cellular activities.
(3) Ions carry
electrical current, which allows production of action potentials and graded
potentials.
(4) Several ions serve as cofactors needed for
optimal activity of enzymes.
Concentrations of Electrolytes in Body Fluids
To compare the
charge carried by ions in different solutions, the concentration of ions is
typically expressed in units of milli equivalents per liter (mEq/liter). These
units give the concentration of cations or anions in a given volume of
solution. One equivalent is the positive or negative charge equal to the amount
of charge in one mole of H; a milli equivalent is one- thousandth of an
equivalent. Recall that a mole of a substance is its molecular weight expressed
in grams. For ions such as sodium (Na), potassium (K), and bicarbonate (HCO3),
which have a single positive or negative charge, the number of mEq/liter is
equal to the number of mmol/liter. For ions such as calcium (Ca2) or phosphate
(HPO42), which have two positive or negative charges, the number of mEq/liter
is twice the number of mmol/liter. Compares the concentrations of the main electrolytes
and protein anions in blood plasma, interstitial fluid, and intracellular fluid.
The chief difference between the two extracellular fluids—blood plasma and
interstitial fluid—is that blood plasma contains many protein anions, in
contrast to interstitial fluid, which has very few. Because normal capillary
membranes are virtually impermeable to proteins, only a few plasma proteins
leak out of blood vessels into the interstitial fluid. This difference in
protein concentration is largely responsible for the blood colloid osmotic
pressure exerted by blood plasma. In other respects, the two fluids are similar.
The electrolyte content of intracellular fluid differs consider- ably from that
of extracellular fluid. In extracellular fluid, the most abundant cation is Na,
and the most abundant anion is Cl. In intracellular fluid, the most abundant cation
is K, and the most abundant anions are proteins and phosphates (HPO42). By
actively transporting Na out of cells and K into cells, sodium–potassium pumps
(Na/K ATPase) play a major role in maintaining the high intracellular
concentration of K and high extracellular concentration of Na.
Sodium ions
(Na) are the most abundant ions in extracellular fluid, accounting for 90% of
the extracellular cations. The normal blood plasma Na concentration is 136–148
mEq/liter. As we have already seen, Na plays a pivotal role in fluid and
electrolyte balance because it accounts for almost half of the osmolarity of
extracellular fluid (142 of about 300 mOsm/liter). The flow of Na through
voltage-gated channels in the plasma membrane also is necessary for the generation
and conduction of action potentials in neurons and muscle fibers. The typical
daily intake of Na in North America often far exceeds the body’s normal daily
requirements, due largely to excess dietary salt the kidneys excrete excess Na,
but they also can conserve it during periods of shortage. The Na level in the
blood is controlled by aldosterone, antidiuretic hormone (ADH), and atrial
natriuretic peptide (ANP). Aldosterone increases renal reabsorption of Na. When
the blood plasma concentration of Na drops below 135 mEq/liter, a condition
called hyponatremia, ADH release ceases. The lack of ADH in turn permits
greater excretion of water in urine and restoration of the normal Na level in
ECF. Atrial natriuretic peptide (ANP) increases Na excretion by the kidneys
when Na level is above normal, a condition called hypernatremia.
Chloride ions
(Cl) are the most prevalent anions in extracellular fluid. The normal blood
plasma Cl concentration is 95–105 mEq/liter. Cl moves relatively easily between
the extracellular and intracellular compartments because most plasma membranes
contain many Cl leakage channels and antiporters. For this reason, Cl can help
balance the level of anions in different fluid compartments. One example is the
chloride shift that occurs between red blood cells and blood plasma as the
blood level of carbon dioxide either increases or decreases. In this case, the
antiporter exchange of Cl for HCO3 maintains the correct balance of anions between
ECF and ICF. Chloride ions also are part of the hydrochloric acid secreted into
gastric juice. ADH helps regulate Cl balance in body fluids because it governs
the extent of water loss in urine. Processes that increase or decrease renal
reabsorption of sodium ions also affect reabsorption of chloride ions. (Recall
that reabsorption of Na and Cl occurs by means of Na Cl symporters.)
Potassium ions
(K) are the most abundant cations in intracellular fluid (140 mEq/liter). K plays
a key role in establishing the resting membrane potential and in the
repolarization phase of action potentials in neurons and muscle fibers; K also
helps maintain normal intracellular fluid volume. When K moves into or out of
cells, it often is exchanged for H and thereby helps regulate the pH of body
fluids. The normal blood plasma K concentration is 3.5– 5.0 mEq/liter and is
controlled mainly by aldosterone. When blood plasma K concentration is high,
more aldosterone is secreted into the blood. Aldosterone then stimulates
principal cells of the renal collecting ducts to secrete more K so excess K is
lost in the urine. Conversely, when blood plasma K concentration is low,
aldosterone secretion decreases and less K is excreted in urine. Because K is
needed during the repolarization phase of action potentials, abnormal K levels
can be lethal. For instance, hyperkalemia (above-normal concentration of K in
blood) can cause death due to ventricular fibrillation.
Bicarbonate
ions (HCO3) are the second most prevalent extracellular anions. Normal blood
plasma HCO3 concentration is 22–26 mEq/liter in systemic arterial blood and
23–27 mEq/ liter in systemic venous blood. HCO3 concentration increases as
blood flows through systemic capillaries because the carbon dioxide released by
metabolically active cells combines with water to form carbonic acid; the
carbonic acid then dissociates into H and HCO3. As blood flows through pulmonary
capillaries, however, the concentration of HCO3 decreases again as carbon
dioxide is exhaled. Intracellular fluid also contains a small amount of HCO3. As
previously noted, the exchange of Cl for HCO3 helps maintain the correct
balance of anions in extracellular fluid and intracellular fluid. The kidneys are
the main regulators of blood HCO3 concentration. The intercalated cells of the
renal tubule can either form HCO3 and release it into the blood when the blood
level is low or excrete excess HCO3 in
the urine when the level in blood is too high. Changes in the blood level of
HCO3 are considered later in this chapter in the section on acid–base balance.
Calcium
Because such a
large amount of calcium is stored in bone, it is the most abundant mineral in
the body. About 98% of the calcium in adults is located in the skeleton and
teeth, where it is combined with phosphates to form a crystal lattice of
mineral salts. In body fluids, calcium is mainly an extracellular cation (Ca2).
The normal concentration of free or unattached Ca2 in blood plasma is 4.5–5.5
mEq/liter. About the same amount of Ca2 is attached to various plasma proteins.
Besides contributing to the hardness of bones and teeth, Ca2 plays important
roles in blood clotting, neurotransmitter release, maintenance of muscle tone,
and excitability of nervous and muscle tissue. The most important regulator of
Ca2 concentration in blood plasma is parathyroid hormone (PTH). A low level of
Ca2 in blood plasma promotes release of more PTH, which stimulates osteoclasts
in bone tissue to release calcium (and phosphate) from bone extracellular
matrix. Thus, PTH increases bone resorption. Parathyroid hormone also enhances
reabsorption of Ca2 from glomerular filtrate through renal tubule cells and back
into blood, and increases production of calcitriol (the form of vitamin D that
acts as a hormone), which in turn increases Ca2 absorption from food in the
gastrointestinal tract. Recall that calcitonin (CT) produced by the thyroid
gland inhibits the activity of osteoclasts, accelerates Ca2 deposition into
bones, and thus lowers blood Ca2 levels.
Phosphate
About 85% of
the phosphate in adults is present as calcium phosphate salts, which are
structural components of bone and teeth. The remaining 15% is ionized. Three
phosphate ions (H2PO4, HPO42, and PO43) are important intracellular anions. At
the normal pH of body fluids, HPO42 is the most prevalent form. Phosphates
contribute about 100 mEq/liter of anions to intracellular fluid. HPO42 is an
important buffer of H, both in body fluids and in the urine. Although some are
“free,” most phosphate ions are covalently bound to organic molecules such as
lipids (phospholipids), proteins, carbohydrates, nucleic acids (DNA and RNA),
and adenosine triphosphate (ATP). The normal blood plasma concentration of
ionized phosphate is only 1.7–2.6 mEq/liter. The same two hormones that govern
calcium homeostasis—parathyroid hormone (PTH) and calcitriol—also regulate the
level of HPO42 in blood plasma. PTH stimulates resorption of bone extracellular
matrix by osteoclasts, which releases both phosphate and calcium ions into the
blood- stream. In the kidneys, however, PTH inhibits reabsorption of phosphate
ions while stimulating reabsorption of calcium ions by renal tubular cells. Thus,
PTH increases urinary excretion of phosphate and lowers blood phosphate level.
Calcitriol promotes absorption of both phosphates and calcium from the
gastrointestinal tract. Fibroblast growth factor 23 (FGF 23) is a polypeptide
paracrine (local hormone) that also helps regulate blood plasma levels of HPO42.
This hormone decreases HPO42 blood
levels by increasing HPO42 excretion by
the kidneys and decreasing absorption of HPO42 by the gastrointestinal tract.
Magnesium
In adults,
about 54% of the total body magnesium is part of bone matrix as magnesium
salts. The remaining 46% occurs as magnesium ions (Mg2) in intracellular fluid
(45%) and extra- cellular fluid (1%). Mg2 is the second most common intracellular
cation (35 mEq/liter). Functionally, Mg2 is a cofactor for certain enzymes
needed for the metabolism of carbohydrates and proteins and for the
sodium–potassium pump. Mg2 is essential for normal neuromuscular activity,
synaptic transmission, and myocardial functioning. In addition, secretion of
parathyroid hormone (PTH) depends on Mg2. Normal blood plasma Mg2 concentration is low,
only 1.3–2.1 mEq/liter. Several factors regulate the blood plasma level of Mg2 by
varying the rate at which it is excreted in the urine. The kidneys increase
urinary excretion of Mg2 in response to hypercalcemia, hypomagnesaemia,
increases in extracellular fluid volume, decreases in parathyroid hormone, and
acidosis. The opposite conditions decrease renal excretion of Mg2. People at
risk for fluid and electrolyte imbalances include those who depend on others for
fluid and food, such as infants, the elderly, and the hospitalized; individuals
undergoing medical treatment that involves intravenous infusions, drainages or
suctions, and urinary catheters; and people who receive diuretics, experience
excessive fluid losses and require increased fluid intake, or experience fluid
retention and have fluid restrictions. Finally, athletes and military personnel
in extremely hot environments, postoperative individuals, severe burn or trauma
cases, individuals with chronic diseases (congestive heart failure, diabetes,
chronic obstructive lung disease, and cancer), people in confinement, and
individuals with altered levels of conscious- ness who may be unable to
communicate needs or respond to thirst are also subject to fluid and electrolyte
imbalances.
ACID–BASE BALANCE
From our
discussion thus far, it should be clear that various ions play different roles
that help maintain homeostasis. A major homeostatic challenge is keeping the H concentration
(pH) of body fluids at an appropriate level. This task—the maintenance of
acid–base balance—is of critical importance to normal cellular function. For
example, the three-dimensional shape of all body proteins, which enable them to
perform specific functions, is very sensitive to pH changes. When the diet
contains a large amount of protein, as is typical in North America, cellular
metabolism produces more acids than bases, which tends to acidify the blood.
Before proceeding with this section of the chapter, you may wish to review the
discussion of acids, bases, and pH on pages 41–43. In a healthy person, several
mechanisms help maintain the pH of systemic arterial blood between 7.35 and 7.45.
(A pH of 7.4 corresponds to an H concentration of 0.00004 mEq/liter 40 nEq
/liter.) Because metabolic reactions often produce a huge excess of H, the lack
of any mechanism for the disposal of H would cause H level in body fluids to rise quickly to a lethal
level. Homeostasis of H concentration within a narrow range is thus essential
to survival. The removal of H from body fluids and its subsequent elimination
from the body depend on the following three major mechanisms:
1. Buffer
systems. Buffers act quickly to temporarily bind H, removing the highly
reactive, excess H from solution. Buffers thus raise pH of body fluids but do
not remove H from the body.
2. Exhalation of carbon dioxide. By increasing
the rate and depth of breathing, more carbon dioxide can be exhaled. Within
minutes this reduces the level of carbonic acid in blood, which raises the
blood pH (reduces blood H level).
3. Kidney
excretion of H. The slowest mechanism, but the only way to eliminate acids
other than carbonic acid, is through their excretion in urine.
The Actions of Buffer
Systems
Most buffer
systems in the body consist of a weak acid and the salt of that acid, which
functions as a weak base. Buffers prevent rapid, drastic changes in the pH of
body fluids by converting strong acids and bases into weak acids and weak bases
within fractions of a second. Strong acids lower pH more than weak acids
because strong acids release H more readily and thus contribute more free
hydrogen ions. Similarly, strong bases raise pH more than weak ones. The
principal buffer systems of the body fluids are the protein buffer system, the
carbonic acid–bicarbonate buffer system, and the phosphate buffer system.
Protein Buffer System
The protein
buffer system is the most abundant buffer in intra- cellular fluid and blood
plasma. For example, the protein hemoglobin is an especially good buffer within
red blood cells, and albumin is the main protein buffer in blood plasma.
Proteins are composed of amino acids, organic molecules that contain at least
one carboxyl group (HCOOH) and at least one amino group (NH2); these groups are
the functional components of the protein buffer system. The free carboxyl group
at one end of a protein acts like an acid by releasing H when pH rises; it
dissociates as follows: a.a COOH group
into coo- and h+…..
The H is then
able to react with any excess OH in the solution to form water. The free amino
group at the other end of a protein can act as a base by combining with H when
pH falls, as follows:
Accept of h+ by
nh2 to become nh3+…….
So proteins
can buffer both acids and bases. In addition to the terminal carboxyl and amino
groups, side chains that can buffer H are present on seven of the 20 amino
acids.
As we have
already noted, the protein hemoglobin is an important buffer of H in red blood
cells (see Figure 23.23 on page 904). As blood flows through the systemic
capillaries, carbon dioxide (CO2) passes from tissue cells into red blood
cells, where it combines with water (H2O) to form carbonic acid (H2CO3). Once
formed, H2CO3 dissociates into H and HCO3. At the same time that CO2 is entering red
blood cells, oxyhemoglobin (Hb.O2) is giving up its oxygen to tissue cells.
Reduced hemoglobin (deoxyhemoglobin) picks up most of the H. For this reason, reduced hemoglobin usually is
written as Hb.H. The following reactions summarize these relations:
H2O + CO2 H2CO3
Water+ Carbon dioxide Carbonic acid
(Entering RBCs) H2CO3
H + HCO3 Carbonic acid Hydrogen ion Bicarbonate ion
Hb–O2 + H Hb–H + O2 Oxyhemoglobin + Hydrogen ion Reduced hemoglobin + Oxygen (released to
tissue cells)
Carbonic Acid–Bicarbonate Buffer System
The carbonic acid–bicarbonate buffer system is
based on the bicarbonate ion (HCO3), which can act as a weak base, and carbonic
acid (H2CO3), which can act as a weak acid. As you have already learned, HCO3 is
a significant anion in both intracellular and extracellular fluids (see Figure
27.6). Because the kidneys also synthesize new HCO3 and reabsorb filtered HCO3,
this important buffer is not lost in the urine. If there is an excess of H, the
HCO3, can function as a weak base and remove the excess H as follows:
H + HCO3 H2CO3 Hydrogen ion + Bicarbonate ion (weak base) Carbonic acid
Then, H2CO3
dissociates into water and carbon dioxide, and the CO2 is exhaled from the
lungs. Conversely, if there is a shortage of H, the H2CO3 can function as a
weak acid and provide H as follows:
H2CO3
H + HCO3 Carbonic acid (weak acid) Hydrogen ion + Bicarbonate ion
At a pH of 7.4, HCO3 concentration is about 24
mEq/liter and H2CO3 concentration is about 1.2 mmol/liter, so bicarbonate ions
outnumber carbonic acid molecules by 20 to 1. Because CO2 and H2O combine to
form H2CO3, this buffer system cannot protect against pH changes due to
respiratory problems in which there is an excess or shortage of CO2.
Phosphate Buffer System
The phosphate buffer system acts via a
mechanism similar to the one for the carbonic acid–bicarbonate buffer system.
The components of the phosphate buffer system are the ions dihydrogen phosphate
(H2PO4) and monohydrogen phosphate (HPO42). Recall that phosphates are major anions in
intracellular fluid and minor ones in extracellular fluids (Figure 27.6). The
dihydrogen phosphate ion acts as a weak acid and is capable of buffering strong
bases such as OH, as follows:
OH + H2PO4 H2O + HPO42
Hydroxide ion (strong base) + Dihydrogen phosphate
(weak acid) Water + Monohydrogen
phosphate (weak base)
The
monohydrogen phosphate ion is capable of buffering the H released by a strong
acid such as hydrochloric acid (HCl) by acting as a weak base:
H + HPO42 H2PO4
Hydrogen ion(strong acid) + Monohydrogen phosphate (weak base) gives
Dihydrogen phosphate (weak acid)
Because the
concentration of phosphates is highest in intra- cellular fluid, the phosphate
buffer system is an important regulator of pH in the cytosol. It also acts to a
smaller degree in extracellular fluids and buffers acids in urine. H2PO42 is
formed when excess H in the kidney tubule fluid combines with HPO42. The H that
becomes part of the H2PO4 passes into the urine. This reaction is one way the
kidneys help maintain blood pH by excreting H in the urine.
Exhalation of Carbon Dioxide
The simple act
of breathing also plays an important role in maintaining the pH of body fluids.
An increase in the carbon dioxide (CO2) concentration in body fluids increases H
concentration and thus lowers the pH (makes body fluids more acidic). Because
H2CO3 can be eliminated by exhaling CO2, it is called a volatile acid.
Conversely, a decrease in the CO2 concentration of body fluids raises the pH
(makes body fluids more alkaline). This chemical interaction is illustrated by
the following reversible reactions:
CO2 + H2O
H 2CO3 H + HCO3 Carbon dioxide
Water Carbonic acid Hydrogen & Bicarbonate ion
Changes in the
rate and depth of breathing can alter the pH of body fluids within a couple of minutes.
With increased ventilation, more CO2 is exhaled. When CO2 levels decrease, the
reaction is driven to the left (blue arrows), H concentration falls, and blood
pH increases. Doubling the ventilation increases pH by about 0.23 units, from
7.4 to 7.63. If ventilation is slower than normal, less carbon dioxide is
exhaled. When CO2 levels increase, the reaction is driven to the right (red
arrows), the H concentration increases, and blood pH decreases. Reducing ventilation
to one-quarter of normal lowers the pH by 0.4 units, from 7.4 to 7.0. These
examples show the powerful effect of alterations in breathing on the pH of body
fluids. The pH of body fluids and the rate and depth of breathing interact via a
negative feedback loop (Figure 27.7). When the blood acidity increases, the decrease
in pH (increase in concentration of H is
detected by central chemoreceptors in the medulla oblongata and peripheral
chemoreceptors in the aortic and carotid bodies, both of which stimulate the
inspiratory area in the medulla oblongata. As a result, the diaphragm and other
respiratory muscles contract more forcefully and frequently, so more CO2 is
exhaled. As less H2CO3 forms and fewer H are present, blood pH increases. When
the response brings blood pH (H concentration) back to normal, there is a
return to acid–base homeostasis. The same negative feedback loop operates if
the blood level of CO2 increases. Ventilation increases, which remove more CO2,
reducing the H concentration and increasing the blood’s pH. By contrast, if the
pH of the blood increases, the respiratory center is inhibited and the rate and
depth of breathing decreases. A decrease in the CO2 concentration of the blood
has the same effect. When breathing decreases, CO2 accumulates in the blood so
its H concentration increases.
Kidney Excretion of H
Metabolic
reactions produce nonvolatile acids such as sulfuric acid at a rate of about 1
mEq of H per day for every kilogram of body mass. The only way to eliminate
this huge acid load is to excrete H in the urine. Given the magnitude of these
contributions to acid–base balance, it’s not surprising that renal failure can
quickly cause death. As you learned in Chapter 26, cells in both the proximal
convoluted tubules (PCT) and the collecting ducts of the kidneys secrete
hydrogen ions into the tubular fluid. In the PCT, Na/H antiporters secrete H as
they reabsorb Na. Even more important for regulation of pH of body fluids,
however, are the intercalated cells of the collecting duct. The apical membranes
of some intercalated cells include proton pumps (HATPases) that secrete H into
the tubular fluid. Intercalated cells can secrete H against a concentration gradient so
effectively that urine can be up to 1000 times (3 pH units) more acidic than
blood. HCO3 produced by dissociation of H2CO3 inside intercalated cells crosses
the basolateral membrane by means of Cl/HCO3 antiporters and then diffuses into
peritubular capillaries. The HCO3 that enters the blood in this way is new (not
filtered). For this reason, blood leaving the kidney in the renal vein may have
a higher HCO3 concentration than blood entering the kidney in the renal artery.
Interestingly, a second type of intercalated cell has proton pumps in its basolateral
membrane and Cl/HCO3 antiporters in its apical membrane. These intercalated
cells secrete HCO3 and reabsorb H. Thus,
the two types of intercalated cells help maintain the pH of body fluids in two
ways—by excreting excess H when pH of
body fluids is too low and by excreting excess HCO3 when pH is too high. Some H secreted into the
tubular fluid of the collecting duct is buffered, but not by HCO3, most of which
has been filtered and reabsorbed. Two other buffers combine with H in the collecting
duct. The most plentiful buffer in the tubular fluid of the collecting duct is
HPO42 (monohydrogen phosphate ion). In addition, a small amount of NH3
(ammonia) also is present. H combines with HPO42 to form H2PO4 (di- hydrogen
phosphate ion) and with NH3 to form NH4 (ammonium ion). Because these ions cannot
diffuse back into tubule cells, they are excreted in the urine.
Acid–Base Imbalances:
The normal pH range of systemic arterial blood is between 7.35 (45 nEq
of H /liter) and 7.45 (35 nEq of H/liter). Acidosis (or acidemia) is a
condition in which blood pH is below 7.35; alkalosis (or alkalemia) is a
condition in which blood pH is higher than 7.45. The major physiological effect
of acidosis is depression of the central nervous system through depression of
synaptic transmission. If the systemic arterial blood pH falls below 7,
depression of the nervous system is so severe that the individual becomes
disoriented, then comatose, and may die. Patients with severe acidosis usually die
while in a coma. A major physiological effect of alkalosis, by contrast, is
over excitability in both the central nervous system and peripheral nerves.
Neurons conduct impulses repetitively, even when not stimulated by normal
stimuli; the results are nervousness, muscle spasms, and even convulsions and
death. A change in blood pH that leads to acidosis or alkalosis may be
countered by compensation, the physiological response to an acid–base imbalance
that acts to normalize arterial blood pH. Compensation may be either complete,
if pH indeed is brought within the normal range, or partial, if systemic
arterial blood pH is still lower than 7.35 or higher than 7.45. If a person has
altered blood pH due to metabolic causes, hyperventilation or hypoventilation
can help bring blood pH back toward the normal range; this form of compensation,
termed respiratory compensation, occurs within minutes and reaches its maximum
within hours. If, however, a person has altered blood pH due to respiratory
causes, then renal compensation—changes in secretion of H and reabsorption of
HCO3 by the kidney tubules—can help reverse the change. Renal compensation may
begin in minutes, but it takes days to reach maximum effectiveness. In the
discussion that follows, note that both respiratory acidosis and respiratory
alkalosis are disorders resulting from changes in the partial pressure of CO2
(PCO2) in systemic arterial blood (normal range is 35–45 mmHg). By contrast,
both metabolic acidosis and metabolic alkalosis are disorders resulting from
changes in HCO3 concentration (normal range is 22–26 mEq/liter in systemic
arterial blood).
Respiratory Acidosis
The hallmark of respiratory acidosis is an
abnormally high PCO2 in systemic arterial blood—above 45 mmHg. Inadequate
exhalation of CO2 causes the blood pH to drop. Any condition that decreases the
movement of CO2 from the blood to the alveoli of the lungs to the atmosphere
causes a buildup of CO2, H2CO3, and H. Such conditions include emphysema, pulmonary
edema, injury to the respiratory center of the medulla oblongata, airway
obstruction, or disorders of the muscles involved in breathing. If the
respiratory problem is not too severe, the kidneys can help raise the blood pH
into the normal range by increasing excretion of H and reabsorption of HCO3
(renal compensation). The goal in treatment of respiratory acidosis is to
increase the exhalation of CO2, as, for instance, by providing ventilation
therapy. In addition, intravenous administration of HCO3 may be helpful.
Respiratory Alkalosis
In respiratory alkalosis, systemic arterial
blood PCO2 falls below 35 mmHg. The cause of the drop in PCO2 and the resulting
increase in pH is hyperventilation, which occurs in conditions that stimulate
the inspiratory area in the brain stem. Such conditions include oxygen deficiency
due to high altitude or pulmonary disease, cerebrovascular accident (stroke),
or severe anxiety. Again, renal compensation may bring blood pH into the normal
range if the kidneys are able to decrease excretion of H and reabsorption of
HCO3. Treatment of respiratory alkalosis is aimed at increasing the level of
CO2 in the body. One simple treatment is to have the person inhale and exhale
into a paper bag for a short period; as a result, the person inhales air
containing a higher-than-normal concentration of CO2.
Metabolic Acidosis
In metabolic acidosis, the systemic arterial
blood HCO3 level drops below 22 mEq/liter. Such a decline in this important
buffer causes the blood pH to decrease. Three situations may lower the blood
level of HCO3 (1) actual loss of HCO3,
such as may occur with severe diarrhea or renal dysfunction; (2) accumulation
of an acid other than carbonic acid, as may occur in ketosis; or (3) failure of
the kidneys to excrete H, from metabolism of dietary proteins. If the problem
is not too severe, hyperventilation can help bring blood pH into the normal
range (respiratory compensation). Treatment of metabolic acidosis consists of
administering intra- venous solutions of sodium bicarbonate and correcting the
cause of the acidosis.
Metabolic Alkalosis
In metabolic alkalosis, the systemic arterial
blood HCO3 concentration is above 26 mEq/liter. A non-respiratory loss of acid
or excessive intake of alkaline drugs causes the blood pH to increase above
7.45. Excessive vomiting of gastric contents, which results in a substantial
loss of hydrochloric acid, is probably the most frequent cause of metabolic
alkalosis. Other causes include gastric suctioning, use of certain diuretics,
endocrine disorders, excessive intake of alkaline drugs (antacids), and severe
dehydration. Respiratory compensation through hypoventilation may bring blood
pH into the normal range. Treatment of metabolic alkalosis consists of giving
fluid solutions to correct Cl, K, and other electrolyte deficiencies plus
correcting the cause of alkalosis.
Composition of urine
Urine is approximately 95% water. The other components of normal urine are the solutes that
are dissolved in the water component of the urine. These solutes can be divided
into two categories according to their chemical structure (e.g. size and
electrical charge).
Organic molecules are electrically neutral and can be relatively large (compared
with the 'simpler' ions - below).
These include:
These include:
- Urea - Urea is an organic (i.e. carbon-based) compound whose chemical formula is: CON2H4 or (NH2)2CO. It is also known as carbamide. Urea is derived from ammonia and produced by the deamination of amino acids. The amount of urea in urine is related to quantity of dietary protein.
- Creatinine - Creatinine is a normal (healthy) constituent of blood. It is produced mainly as a result of the breakdown of creatine phosphate in muscle tissue. It is usually produced by the body at a fairly constant rate (which depends on the muscle mass of the body).
- Uric acid - Uric acid is an organic
(i.e. carbon-based) compound whose chemical formula is: C5H4N4O3.
Due to its insolubility, uric acid has a tendency to crystallize, and is a common part of kidney stones.
Other
substances/molecules - Example of other
substances that may be found in small amounts in normal urine include
carbohydrates, enzymes, fatty acids, hormones, pigments, and mucins (a group of large, heavily
glycosylated proteins found in the body).
Ions are atoms or groups of atoms that have either, lost some
outer electrons, hence have a positive electric charge, or have gained
some outer electrons (to the atom or group of atoms), and hence have a negative
electric charge. Even in the cases of ions formed by groups of atoms (they
are ions due to the few lost or gained electrons), the groups are
formed from only a small number of particles and therefore tend to be
relatively small.
These include:
These include:
Individual elements:
|
|
Small groups formed from a few different elements:
|
|
Nephrosis and nephritis
An inflammation of one or both kidneys is called nephritis.
It is more common in childhood and adolescence. Nephritis most often affects
the glomeruli, tufts of microscopic vessels that filter blood. Less commonly,
nephritis affects the tubules that surround the glomeruli or the blood vessels
inside the kidneys. Nephritis may be acute or chronic. People with the acute
form usually recover. Nephrosis is a non-inflammatory disease of the kidney
also affecting the glomeruli.
Chronic nephritis can lead to severe hypertension which can,
in extreme cases, result in death from kidney or heart failure.
Nephrosis occurs when the glomeruli are damaged; instead of
filtering only wastes and water from the blood, the glomeruli also filter out
protein. Without sufficient protein, a person may develop edema (swelling) in
the feet, ankles, and abdomen and around the eyes. Nephrosis can occur in
people of all ages, but is more common in children.
Symptoms
·
Loss of appetite
·
Fatigue
·
Stomached ache/
abdominal pain
·
Dark urine
·
Facial swelling
·
Edema.
Causes
Acute nephritis: can be caused by drug allergies, especially
analgesic such as aspirin and paracetomol, immunosuppressant drugs such as
cyclosporine, anti-cancer drugs such as cisplatin and carboplatin, and lithium,
which is used to treat bipolar disorder. Other causes include bacterial and
viral infections, metabolic and toxic disorders, and hypocalcaemia.
Chronic nephritis: develops more slowly has many causes,
including abnormal immune system reactions, bacterial kidney infection, drug
hypersensitivity or exposure to a toxin. It can also be caused by radiation
exposure, obstruction of the urinary tract, hypertension, sickle cell anemia
and polycystic kidney disease (PKD), among other conditions.
Nephrosis: can be caused by kidney disease or it may be a
complication of another disorder, particularly diabetes.
The risk factors include:
- History of polycystic kidney disease.
- Kidney disease or infection.
- Drug allergies.
- Hypertension.
- Diabetes.
- Sickle cell anemia.
- Long-term dialysis.
Diagnosis
Common diagnostic tests for nephritis & Nephrosis
include:-
- Urinalysis to check kidney function.
- Renal ultrasounds to check size and shape of the kidneys and to determine whether there are any blockages in the urinary tract.
- Renal
scan may also be done to measure blood flow thought the kidneys.
A biopsy may also be performed.
Treatment
The aim of all treatment is to reduce inflammation, limit
damage to the kidney's, and support the body until kidney function is restored.
- Medication – Nephritis caused by infection is treated with antibiotics. Both nephritis and nephrosis may be treated with anti-inflammatory drugs. Diuretics or special diets may be prescribed. Nephrosis can sometimes be suppressed using corticosteroids, including prednisone and cortisone.
- Dialysis – If either condition progress to kidney failure, dialysis may be needed, which is a treatment that filters wastes from the blood.
- Surgery – For kidney failure, a kidney transplant may be needed.
Tubular
Function Tests
Tests of
renal tubular function can define states of diuresis and antidiuretics and
natriuresis and antinatriuresis. Under certain circumstances the tests can
distinguish oliguria due to pre renal azotemia, which is reversed by
restoration of hemodynamic status to normal, from that due to established acute
renal failure, which persists despite restoration of normal renal blood flow.
In the former, tubular conservation mechanisms are enhanced, and in the latter
they are lost. However, in non oliguric renal dysfunction, which accounts for
more than 50 percent of cases encountered clinically, the differences in
tubular function are less distinct from prerenal azotemia. Diuretic therapy
overcomes tubular conserving function. Thus, treatment with loop diuretics, osmotic
diuretics, saline loading, or natriuretic vasodilators (low-dose dopamine,
fenoldopam, prostaglandin E1, or ANP) may render tubular function tests
uninterpretable.
RELATED PICTURES:
 | |||
| MORPHOLOGY OF KIDNEY |
 |
| ANATOMICAL FEATURES OF KIDNEY |
 |
| ANATOMICAL FEATURES OF KIDNEY |
 |
| STRUCTURE OF NEPHRON |
 |
| COMPOSITION OF NORMAL URINE |
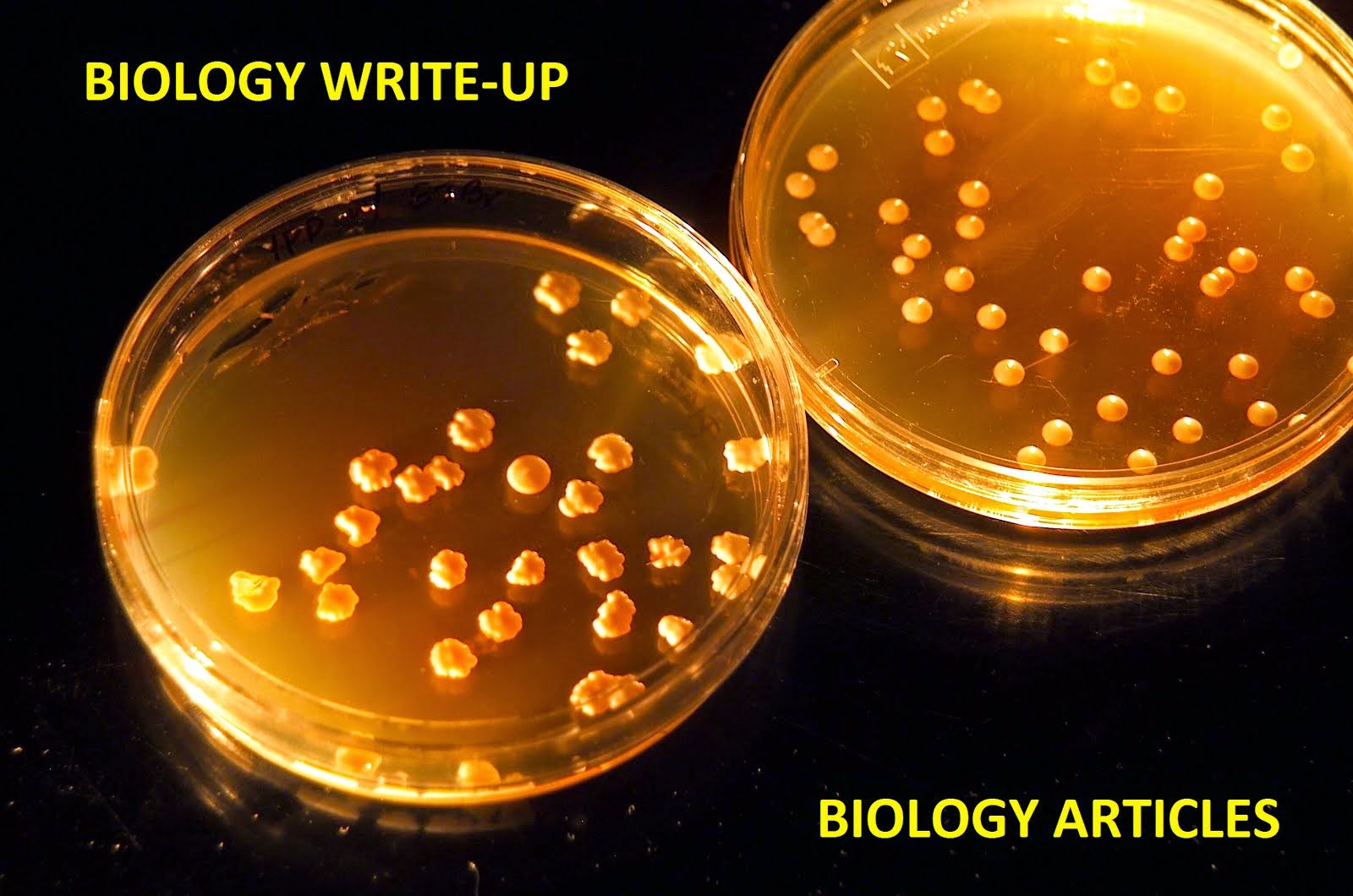
No comments:
Post a Comment