General physiology:
Nervous System
OBJECTIVES
•
Describe the organization of the nervous system.
•
Describe the three basic functions of the nervous system.
Organization
of the Nervous System
The
nervous system is one of the smallest and yet the most complex of the 11 body
systems. This intricate network of billions of neurons and even more neuroglia
is organized into two main subdivisions: the central nervous system and the
peripheral nervous system.
Central
Nervous System:
The central nervous system (CNS) consists of the brain and
spinal cord .The brain is the part of the CNS that is located in the skull and
contains about 100 billion (1011) neurons. The spinal cord is connected to the
brain through the foramen magnum of the occipital bone and is encircled by the
bones of the vertebral column. The spinal cord contains about 100 million
neurons. The CNS processes many different kinds of incoming sensory
information. It is also the source of thoughts, emotions, and memories. Most
signals that stimulate muscles to contract and glands to secrete originate in
the CNS.
Note: CNS has two parts
brain and spinal cord. Axon tracts of pathways run longitudinally through the
spinal cord. Some run down wards and some up wards. Afferent nerve fibers enter
from the dorsal side of spinal cord and are called dorsal root, and form clumps
called as dorsal groove ganglia. The efferent nerve fibers leave the spinal
cord on the ventral side and make ventral roots. They come together and make a
pair of spinal nerves.
Brain
has three parts: fore brain, mid brain and hind brain. Fore brain has cerebrum
and diencephalon. The mid brain, Pons and the medulla forms the brain stem
which extends as the spinal cord. Hind brain has cerebellum. Along the brain
stem, longitudinally relays the nerve fibers (both afferent and efferent). The
small hyaline branched neurons of the core tissue of the brain forms the
reticular formation which cluster and form the brain stem nuclei which is a
integrating center has both ascending system and the descending system. The
ascending system influences the afferent fibers while the descending system
influences the efferent and sometimes also the afferent.
Peripheral
Nervous System:
The peripheral nervous system (PNS) (pe-RIF-e-ral) consists
of all nervous tissue outside the CNS. Components of the PNS include nerves,
ganglia, enteric plexuses, and sensory receptors. A nerve is a bundle of
hundreds to thousands of axons plus associated connective tissue and blood
vessels that lays out- side the brain and spinal cord. Twelve pairs of cranial
nerves emerge from the brain and thirty-one pairs of spinal nerves emerge from
the spinal cord. Each nerve follows a defined path and serves a specific region
of the body. Ganglia (GANG-gle¯-a swelling or knot; singular is ganglion) are
small masses of nervous tissue, consisting primarily of neuron cell bodies,
that are located outside of the brain and spinal cord. Ganglia are closely
associated with cranial and spinal nerves. Enteric plexuses (PLEK-sus-ez) are
extensive networks of neurons located in the walls of organs of the
gastrointestinal tract. The neurons of these plexuses help regulate the
digestive system. The term sensory receptor refers to a structure of the
nervous system that monitors changes in the external or internal environment.
Examples of sensory receptors include touch receptors in the skin,
photoreceptors in the eye, and olfactory receptors in the nose. The PNS is
divided into a somatic nervous system (SNS) (so¯- MAT-ik; soma body), an
autonomic nervous system (ANS) (aw-to¯-NOM-ik; auto- self; -nomic law), and an
enteric nervous system (ENS) (en-TER-ik; enteron intestines). The SNS consists
of (1) sensory neurons that convey information from somatic receptors in the
head, body wall, and limbs and from receptors for the special senses of vision,
hearing, taste, and smell to the CNS and (2) motor neurons that conduct
impulses from the CNS to skeletal muscles only. Because these motor responses
can be consciously controlled, the action of this part of the PNS is voluntary.
The ANS consists of (1) sensory neurons that convey information from autonomic
sensory receptors, located primarily in visceral organs such as the stomach and
lungs, to the CNS and (2) motor neurons that conduct nerve impulses from the
CNS to smooth muscle, cardiac muscle, and glands. Because its motor responses
are not normally under conscious control, the action of the ANS is involuntary.
The motor part of the ANS consists of two branches, the sympathetic division
and the parasympathetic division. With a few exceptions, effectors receive
nerves from both divisions, and usually the two divisions have opposing
actions. For example, sympathetic neurons increase heart rate, and parasympathetic
neurons slow it down. In general, the sympathetic division helps support
exercise of emergency actions, the “fight-or-flight” responses, and the
parasympathetic division takes care of “rest-and-digest” activities. The
operation of the ENS, the “brain of the gut,” is involuntary. Once considered
part of the ANS, the ENS consists of over 100 million neurons in enteric
plexuses that extend most of the length of the gastrointestinal (GI) tract.
Many of the neurons of the enteric plexuses function independently of the ANS
and CNS to some extent, although they also communicate with the CNS via
sympathetic and parasympathetic neurons. Sensory neurons of the ENS monitor
chemical changes within the GI tract as well as the stretching of its walls.
Enteric motor neurons govern contraction of GI tract smooth muscle to propel
food through the GI tract, secretions of the GI tract organs such as acid from
the stomach, and activity of GI tract endocrine cells, which secrete hormones.
The
neurons of the PNS lie outside of the CNS and their clusters are called as the
ganglia. Somatic system controls the skeletal muscles and their axon terminals
release the neurotransmitters into the neuro muscular junction. These neuro
transmitters are generally acetyl choline.
Functions
of the Nervous System
The
nervous system carries out a complex array of tasks. It allows us to sense
various smells, produce speech, and remember past events; in addition, it
provides signals that control body movements and regulates the operation of
internal organs. These diverse activities can be grouped into three basic
functions: sensory (input), integrative (process), and motor (output).
•
Sensory function. Sensory receptors detect internal stimuli, such as an
increase in blood pressure, or external stimuli (for example, a raindrop
landing on your arm). This sensory information is then carried into the brain
and spinal cord through cranial and spinal nerves.
•
Integrative function. The nervous system processes sensory information by
analyzing it and making decisions for appropriate responses—an activity known
as integration.
•
Motor function. Once sensory information is integrated, the nervous system may
elicit an appropriate motor response by activating effectors (muscles and
glands) through cranial and spinal nerves. Stimulation of the effectors causes
muscles to contract and glands to secrete.
The
three basic functions of the nervous system occur, for example, when you answer
your cell phone after hearing it ring. The sound of the ringing cell phone
stimulates sensory receptors in your ears (sensory function). This auditory
information is subsequently relayed into your brain where it is processed and
the decision to answer the phone is made (integrative function). The brain then
stimulates the contraction of specific muscles that will allow you to grab the
phone and press the appropriate button to answer it (motor function).
HISTOLOGY
OF NERVOUS TISSUE
OBJECTIVES
•
Contrast the histological characteristics and the functions of neurons and
neuroglia.
•
Distinguish between gray matter and white matter.
Nervous
tissue comprises two types of cells—neurons and neuroglia. These cells combine
in a variety of ways in different regions of the nervous system. In addition to
forming the complex processing networks within the brain and spinal cord,
neurons also connect all regions of the body to the brain and spinal cord. As
highly specialized cells capable of reaching great lengths and making extremely
intricate connections with other cells, neurons provide most of the unique
functions of the nervous system, such as sensing, thinking, remembering,
controlling muscle activity, and regulating glandular secretions. As a result
of their specialization, they have lost the ability to undergo mitotic
divisions. Neuroglia are smaller cells but they greatly outnumber neurons,
perhaps by as much as 25 times. Neuroglia supports, nourishes, and protects
neurons, and maintain the interstitial fluid that bathes them. Unlike neurons,
neuroglia continue to divide throughout an individual’s lifetime. Both neurons
and neuroglia differ structurally depending on whether they are located in the
central nervous system or the peripheral nervous system. These differences in
structure correlate with the differences in function of the central nervous
system and the peripheral nervous system.
Neurons
Like
muscle cells, neurons (nerve cells) (NOO-rons) possess electrical excitability
(ek-s¯ıt-a-BIL-i-te¯), the ability to respond to a stimulus and convert it into
an action potential. A stimulus is any change in the environment that is strong
enough to initiate an action potential. An action potential (nerve impulse) is
an electrical signal that propagates (travels) along the surface of the
membrane of a neuron. It begins and travels due to the movement of ions (such
as sodium and potassium) between interstitial fluid and the inside of a neuron
through specific ion channels in its plasma membrane. Once begun, a nerve
impulse travels rapidly and at a constant strength. Some neurons are tiny and
propagate impulses over a short distance (less than 1 mm) within the CNS.
Others are the longest cells in the body. The neurons that enable you to wiggle
your toes, for example, extend from the lumbar region of your spinal cord (just
above waist level) to the muscles in your foot. Some neurons are even longer.
Those that allow you to feel a feather tickling your toes stretch all the way
from your foot to the lower portion of your brain. Nerve impulses travel these
great distances at speeds ranging from 0.5 to 130 meters per second (1 to 290
mi/hr).
Parts
of Neuron Most neurons have three parts:
(1) a cell body, (2) dendrites, and
(3) an axon the cell body, also known as the perikaryon (per-i-KAR-e¯-on) or
soma, contains a nucleus surrounded by cytoplasm that includes typical cellular
organelles such as lysosomes, mitochondria, and a Golgi complex. Neuronal cell
bodies also contain free ribosomes and prominent clusters of rough endoplasmic
reticulum, termed Nissl bodies (NIS-el). The ribosomes are the sites of protein
synthesis. Newly synthesized proteins produced by Nissl bodies are used to
replace cellular components, as material for growth of neurons, and to
regenerate damaged axons in the PNS. The cytoskeleton includes both neurofibrils
(noo-ro¯-FI ¯-brils), composed of bundles of intermediate filaments that provide
the cell shape and support, and microtubules (mı¯-kro¯-TOO-bu¯ls), which assist
in moving materials between the cell body and axon. Aging neurons also contain
lipofuscin (l¯ıp-o-FYU ¯S-¯ın), a pigment that occurs as clumps of yellowish
brown granules in the cytoplasm. Lipofuscin is a product of neuronal lysosomes
that accumulates as the neuron ages, but does not seem to harm the neuron as it
ages. A nerve fiber is a general term for any neuronal process (extension) that
emerges from the cell body of a neuron. Most neurons have two kinds of
processes: multiple dendrites and a single axon. Dendrites (DEN-dr¯ıts little
trees) are the receiving or input portions of a neuron. The plasma membranes of
dendrites (and cell bodies) contain numerous receptor sites for binding
chemical messengers from other cells. Dendrites usually are short, tapering,
and highly branched. In many neurons the dendrites form a tree- shaped array of
processes extending from the cell body. Their cytoplasm contains Nissl bodies,
mitochondria, and other organelles. The single axon (axis) of a neuron
propagates nerve impulses toward another neuron, a muscle fiber, or a gland cell.
An axon is a long, thin, cylindrical projection that often joins to the cell
body at a cone-shaped elevation called the axon hillock (HIL- lok small
hill). The part of the axon closest to the axon hillock is the initial segment.
In most neurons, nerve impulses arise at the junction of the axon hillock and
the initial segment, an area called the trigger zone, from which they travel
along the axon to their destination. An axon contains mitochondria,
microtubules, and neurofibrils. Because rough endoplasmic reticulum is not
present, protein synthesis does not occur in the axon. The cytoplasm of an
axon, called axoplasm, is surrounded by a plasma membrane known as the axolemma
(lemma sheath or husk). Along the length of an axon, side branches called axon collaterals
may branch off, typically at a right angle to the axon. The axon and its
collaterals end by dividing into many fine processes called axon terminals
(telodendria) (te¯l-o¯-DEN-dre¯-a). The site of communication between two
neurons or between a neuron and an effector cell is called a synapse (SIN-aps).
The tips of some axon terminals swell into bulb-shaped structures called
synaptic end bulbs; others exhibit a string of swollen bumps called
varicosities (var-i-KOS-i-te¯z). Both synaptic end bulbs and varicosities
contain many tiny membrane-enclosed sacs called synaptic vesicles that store a
chemical called a neurotransmitter (noo-ro¯- trans-MIT-ter). A neurotransmitter
is a molecule released from a synaptic vesicle that excites or inhibits another
neuron, muscle fiber, or gland cell. Many neurons contain two or even three
types of neurotransmitters, each with different effects on the postsynaptic
cell. Because some substances synthesized or recycled in the neuron cell body
are needed in the axon or at the axon terminals, two types of transport systems
carry materials from the cell body to the axon terminals and back. The slower
system, which moves materials about 1–5 mm per day, is called slow axonal
transport. It conveys axoplasm in one direction only—from the cell body toward
the axon terminals. Slow axonal transport supplies new axoplasm to developing
or regenerating axons and replenishes axoplasm in growing and mature axons.
Fast axonal transport, which is capable of moving materials a distance of 200–400
mm per day, uses proteins that function as “motors” to move materials along the
surfaces of microtubules of the neuron’s cytoskeleton. Fast axonal transport
moves materials in both directions—away from and toward the cell body. Fast
axonal transport that occurs in an anterograde (forward) direction moves
organelles and synaptic vesicles from the cell body to the axon terminals. Fast
axonal transport that occurs in a retrograde (backward) direction moves
membrane vesicles and other cellular materials from the axon terminals to the
cell body to be degraded or recycled. Substances that enter the neuron at the
axon terminals are also moved to the cell body by fast retrograde transport.
These substances include trophic chemicals such as nerve growth factor and
harmful agents such as tetanus toxin and the viruses that cause rabies, herpes
simplex, and polio.
Note:
Dendrites conduct
impulse form other neurons meant for reception of the signal. They are just the
branched outgrowths of cell/membrane. Surface area gets increased so as
to receive max. Amount of the impulse.
Axon
has got some divisions: the initial segment:- True electrical signals are
generated here. The axon branches out and they are called as axon collaterals ;
which further branch out and end up as axon terminals.
Chemical
linkage: communication between the neurons occurs by the chemical linkage and
not by physical linkage. Through the axon terminals the neuro transmitters are
released into the synaptic cleft or the junction from where these neuro
transmitters are taken up by the dendrites of other neurons having particular
receptors.
The
neuro transmitters are synthesized by the cell body of the neuron.
Axons
also have some bulges which are called as vericosities.
Neuro
filaments are the cytoskeletal materials which are responsible for the
transportation of the impulse from cell body to the axon. Depending on the
situation and the environment the neuron is exposed it may conduct the opposite
signals and transport it, which changes the metabolic activity of the neuron.
Structural
Diversity in Neurons displays great diversity in size and shape. For example,
their cell bodies range in diameter from 5 micrometers (m) (slightly smaller
than a red blood cell) up to 135 m (barely large enough to see with the unaided
eye). The pattern of dendritic branching is varied and distinctive for neurons
in different parts of the nervous system. A few small neurons lack an axon, and
many others have very short axons. As we have already discussed, the longest
axons are almost as long as a person is tall, extending from the toes to the
lowest part of the brain.
Classification
of Neurons: Both structural and functional features are used to classify the
various neurons in the body.
Based
on the functional features of the neurons they are classified as follows:-
1).
afferent neuron: those neurons which carry the signal from the peripheral
organs to the CNS. Also called as sensory neurons. They either contain sensory
receptors at their distal ends (dendrites) or are located just after sensory
receptors that are separate cells. Once an appropriate stimulus activates a
sensory receptor, the sensory neuron forms an action potential in its axon and
the action potential is conveyed into the CNS through cranial or spinal nerves.
2).
Efferent neurons: those neurons which carry the signal from the CNS to the
peripheral organs. Also called as motor neurons. They convey action potentials
away from the CNS to effectors (muscles and glands) in the periphery (PNS) through
cranial or spinal nerves
3).
Inter neurons: these neurons interlinks between the afferent and efferent
neurons. 99% of the total neurons in our body are inter neurons. Also called as
association neurons. Inter neurons integrate (process) incoming sensory
information from sensory neurons and then elicit a motor response by activating
the appropriate motor neurons. Most interneurons are multipolar in structure
Analogy: For every afferent
neuron there will be 10 efferent neurons and 200,000 inter neurons.
Note:
the first neuron is called as the pre synaptic neuron. The second neuron
which carries the impulse away from the synapse is called as the post synaptic
neuron. The post synaptic neuron may have 1000”s of junctions to receive
impulse from multiple neurons. Not all the junctions are permanent they may be
changing and not all the junctions are active at a time.
Neuroglia
Neuroglia
or glia make up about half the volume of the CNS. Their name derives from the
idea of early histologists that they were the “glue” that held nervous tissue
together. We now know that neuroglia are not merely passive bystanders but
rather actively participate in the activities of nervous tissue. Generally,
neuroglia are smaller than neurons, and they are 5 to 25 times more numerous.
In contrast to neurons, glia do not generate or propagate action potentials,
and they can multiply and divide in the mature nervous system. In cases of
injury or disease, neuroglia multiply to fill in the spaces formerly occupied by
neurons. Brain tumors derived from glia, called gliomas (gle¯-O ¯-mas), tend to
be highly malignant and to grow rapidly. Of the six types of neuroglia,
four—astrocytes, oligodendrocytes, microglia, and ependymal cells—are found
only in the CNS. The remaining two types—Schwann cells and satellite cells—are
present in the PNS.
Neuroglia
of the CNS Neuroglia of the CNS can be classified on the basis of size,
cytoplasmic processes, and intracellular organization into four types:
astrocytes, oligodendrocytes, microglia, and ependymal cells.
ASTROCYTES
These star- shaped
cells have many processes and are the largest and most numerous of the
neuroglia. There are two types of astrocytes. Protoplasmic astrocytes have many
short branching processes and are found in gray matter (described shortly).
Fibrous astrocytes have many long unbranched processes and are located mainly
in white matter (also described shortly). The processes of astrocytes make
contact with blood capillaries, neurons, and the pia mater (a thin membrane
around the brain and spinal cord). The functions of astrocytes include the
following:
(1) Astrocytes contain microfilaments that give them considerable
strength, which enables them to support neurons.
(2) Processes of astrocytes
wrapped around blood capillaries isolate neurons of the CNS from various
potentially harmful substances in blood by secreting chemicals that maintain
the unique selective permeability characteristics of the endothelial cells of
the capillaries. In effect, the endothelial cells create a blood–brain barrier,
which restricts the movement of substances between the blood and interstitial
fluid of the CNS. Details of the blood–brain barrier. In the embryo, astrocytes
secrete chemicals that appear to regulate the growth, migration, and
interconnection among neurons in the brain. (4) Astrocytes help to maintain the
appropriate chemical environment for the generation of nerve impulses. For
example, they regulate the concentration of important ions such as k take up
excess neurotransmitters; and serve as a conduit for the passage of nutrients
and other substances between blood capillaries and neurons.
(5) Astrocytes may
also play a role in learning and memory by influencing the formation of neural synapses.
OLIGODENDROCYTES
These resemble astrocytes but are smaller and contain fewer processes.
Oligodendrocyte processes are responsible for forming and maintaining the
myelin sheath around CNS axons. As you will see shortly, the myelin sheath is a
multilayered lipid and protein covering around some axons that insulates them
and increases the speed of nerve impulse conduction. Such axons are said to be
myelinated.
MICROGLIA
these neuroglia are small cells with slender processes that give off numerous
spine like projections. Microglia function as phagocytes. Like tissue
macrophages, they remove cellular debris formed during normal development of
the nervous system and phagocytize microbes and damaged nervous tissue
EPENDYMAL
CELLS
Ependymal cells are cuboidal to columnar cells arranged in a single
layer that possess microvilli and cilia. These cells line the ventricles of the
brain and central canal of the spinal cord (spaces filled with cerebrospinal
fluid, which protects and nourishes the brain and spinal cord). Functionally,
ependymal cells produce, possibly monitor, and assist in the circulation of
cerebrospinal fluid. They also form the blood–cerebrospinal fluid barrier.
Neuroglia
of the PNS: Neuroglia of the PNS completely surround axons and cell bodies. The
two types of glial cells in the PNS are Schwann cells and satellite cells.
SCHWANN
CELLS (SCHVON or SCHWON)
these cells encircle PNS axons. Like oligodendrocytes,
they form the myelin sheath around axons. However, a single oligodendrocyte
myelinates several axons, but each Schwann cell myelinates a single axon c). A
single Schwann cell can also enclose as many as 20 or more unmyelinated axons
(axons that lack a myelin sheath). Schwann cells participate in axon regeneration,
which is more easily accomplished in the PNS than in the CNS.
SATELLITE
CELLS
These flat cells surround the cell bodies of neurons of PNS ganglia.
Besides pro- viding structural support, satellite cells regulate the exchanges
of materials between neuronal cell bodies and interstitial -fluid.
Myelination
As you have already learned, axons surrounded by a multilayered lipid and
protein covering, called the myelin sheath, are said to be myelinated. The
sheath electrically insulates the axon of a neuron and increases the speed of
nerve impulse conduction. Axons without such a covering are said to be
unmyelinated. Two types of neuroglia produce myelin sheaths: Schwann cells (in
the PNS) and oligodendrocytes (in the CNS). Schwann cells begin to form myelin
sheaths around axons during fetal development. Each Schwann cell wraps about 1
millimeter (1 mm 0.04 in.) of a single axon’s length by spiraling many times
around the axon. Eventually, multiple layers of glial plasma membrane surround
the axon, with the Schwann cell’s cytoplasm and nucleus forming the outermost
layer. The inner portion, consisting of up to 100 layers of Schwann cell
membrane, is the myelin sheath. The outer nucleated cytoplasmic layer of the
Schwann cell, which encloses the myelin sheath, is the neurolemma (sheath of
Schwann). A neurolemma is found only around axons in the PNS. When an axon is
injured, the neurolemma aids regeneration by forming a regeneration tube that
guides and stimulates regrowth of the axon. Gaps in the myelin sheath, called
nodes of Ranvier appear at intervals along the axon. Each Schwann cell wraps
one axon segment between two nodes. In the CNS, an oligodendrocyte myelinates
parts of several axons. Each oligodendrocyte puts forth about 15 broad, flat
processes that spiral around CNS axons, forming a myelin sheath. A neurolemma
is not present, however, because the oligodendrocyte cell body and nucleus do
not envelop the axon. Nodes of Ranvier are present, but they are fewer in
number. Axons in the CNS display little regrowth after injury. This is thought
to be due, in part, to the absence of a neurolemma, and in part to an
inhibitory influence exerted by the oligodendrocytes on axon regrowth. The
amount of myelin increases from birth to maturity, and its presence greatly
increases the speed of nerve impulse conduction. An infant’s responses to
stimuli are neither as rapid nor as coordinated as those of an older child or
an adult, in part because myelination is still in progress during infancy.
Clusters
of Neuronal Cell Bodies Recall that a ganglion (plural is ganglia) refers to a
cluster of neuronal cell bodies located in the PNS. As mentioned earlier,
ganglia are closely associated with cranial and spinal nerves. By contrast, a
nucleus is a cluster of neuronal cell bodies located in the CNS.
Composition
and function of myelin sheath
Myelin is a
dielectric (electrically insulating) material that forms a layer, the myelin
sheath, usually around only the axon of a neuron. It is essential for the
proper functioning of the nervous system. It is an outgrowth of a type of glial
cell. The production of the myelin sheath is called myelination. In humans, the
production of myelin begins in the 14th week of fetal development, although
little myelin exists in the brain at the time of birth. During infancy,
myelination occurs quickly and continues through the adolescent stages of life.
Schwann cells supply the myelin for
peripheral neurons, whereas oligodendrocytes, specifically of the
interfascicular type, myelinate the axons of the central nervous system. Myelin
is considered a defining characteristic of the (gnathostome) vertebrates, but
myelin-like sheaths have also arisen by parallel evolution in some
invertebrates, although they are quite different from vertebrate myelin at the
molecular level. Myelin was discovered in 1854 by Rudolf Virchow.
Myelin is made up by different cell
types, and varies in chemical composition and configuration, but performs the
same insulating function. Myelinated axons are white in appearance, hence the
"white matter" of the brain. The fat helps to insulate the axons from
electrically charged atoms and molecules. These charged particles (ions) are
found in the fluid surrounding the entire nervous system. Under a microscope,
myelin looks like strings of sausages. Myelin is also a part of the maturation
process leading to a child's fast development, including crawling and walking
in the first year.
Myelin
is about 40% water; the dry mass is about 70 - 85% lipids and about 15 - 30%
proteins. Some of the proteins are myelin basic protein, myelin oligodendrocyte
glycoprotein, and proteolipid protein. The primary lipid of myelin is a
glycolipid called galactocerebroside. The intertwining hydrocarbon chains of
sphingomyelin serve to strengthen the myelin sheath.
The
main purpose of a myelin layer (or sheath) is to increase the speed at which
impulses propagate along the myelinated fiber. Along unmyelinated fibers,
impulses move continuously as waves, but in myelinated fibers, they hop or
"propagate by saltation." Myelin decreases capacitance across the
cell membrane, and increases electrical resistance. Thus, myelination helps
prevent the electrical current from leaving the axon. It has been suggested
that myelin permits larger body size by maintaining agile communication between
distant body parts.
When
a peripheral fiber is severed, the myelin sheath provides a track along which
regrowth can occur. Unfortunately, the myelin layer does not ensure a perfect
regeneration of the nerve fiber. Some regenerated nerve fibers do not find the
correct muscle fibers and some damaged motor neurons of the peripheral nervous
system die without regrowth. Damage to the myelin sheath and nerve fiber is
often associated with increased functional insufficiency.
Unmyelinated
fibers and myelinated axons of the mammalian central nervous system do not
regenerate.
Some
studies have revealed optic nerve fibers can be regenerated in postnatal rats.
This regeneration depends upon two conditions: axonal die-back has to be
prevented with appropriate neurotrophic factors and neurite growth inhibitory
components have to be inactivated. These studies may lead to further
understanding of nerve fiber regeneration in the central nervous system.
Review:
Overview of the Nervous System
1. The central nervous system (CNS) consists of
the brain and spinal cord.
2. The peripheral nervous system (PNS) consists of
all nervous tissue outside the CNS. Components of the PNS include nerves,
ganglia, enteric plexuses, and sensory receptors.
3. The PNS is divided into a
somatic nervous system (SNS), autonomic nervous system (ANS), and enteric
nervous system (ENS).
4. The SNS consists of sensory neurons that conduct
impulses from somatic and special sense receptors to the CNS and motor neurons
from the CNS to skeletal muscles.
5. The ANS contains sensory neurons from
visceral organs and motor neurons that convey impulses from the CNS to smooth
muscle tissue, cardiac muscle tissue, and glands.
6. The ENS consists of
neurons in enteric plexuses in the gastrointestinal (GI) tract that function
some- what independently of the ANS and CNS. The ENS monitors chemical changes
within the GI tract and stretching of its walls; the ENS also controls
contraction of GI tract smooth muscle.
7. The nervous system helps maintain
homeostasis and integrates all body activities by sensing changes (sensory
function), interpreting them (integrative function), and reacting to them
(motor function).
Histology
of Nervous Tissue .
Nervous tissue consists of neurons (nerve cells) and neuroglia.
Neurons have the property of electrical excitability and are responsible for
most unique functions of the nervous system:
1. sensing, thinking, remembering,
controlling muscle activity, and regulating glandular secretions.
2. Most
neurons have three parts. The dendrites are the main receiving or input region.
Integration occurs in the cell body, which includes typical cellular
organelles. The output part typically is a single axon, which propagates nerve
impulses toward another neuron, a muscle fiber, or a gland cell.
3. Synapses are
the site of functional contact between two excitable cells. Axon terminals
contain synaptic vesicles filled with neurotransmitter molecules.
4. Slow axonal
transport and fast axonal transport are systems for conveying materials to and
from the cell body and axon terminals.
5. On the basis of their structure,
neurons are classified as multipolar, bipolar, or unipolar.
6. Neurons are
functionally classified as sensory (afferent) neurons, motor (efferent) neurons,
and interneurons. Sensory neurons carry sensory information into the CNS. Motor
neurons carry information out of the CNS to effectors (muscles and glands).
Interneurons are located within the CNS between sensory and motor neurons.
7.
Neuroglia support, nurture, and protect neurons and maintain the interstitial
fluid that bathes them. Neuroglia in the CNS include astrocytes,
oligodendrocytes, microglia, and ependymal cells. Neuroglia in the PNS include
Schwann cells and satellite cells.
8. Two types of neuroglia produce myelin
sheaths: Oligodendrocytes myelinate axons in the CNS, and Schwann cells
myelinate axons in the PNS.
9. White matter consists of aggregates of
myelinated axons; gray matter contains cell bodies, dendrites, and axon
terminals of neurons, unmyelinated axons, and neuroglia.
10. In the spinal
cord, gray matter forms an H-shaped inner core that is surrounded by white
matter in the brain, a thin; superficial shell of gray matter covers the
cerebral and cerebellar hemispheres.
ELECTRICAL
SIGNALS IN NEURONS
OBJECTIVES
•
Describe the cellular properties that permit communication among neurons and
effectors.
•
Compare the basic types of ion channels, and explain how they relate to graded
potentials and action potentials.
•
Describe the factors that maintain a resting membrane potential.
•
List the sequence of events that generate an action potential.
Like
muscle fibers, neurons are electrically excitable. They communicate with one
another using two types of electrical signals: (1) Graded potentials are used
for short-distance communication only.
(2) Action potentials allow
communication over long distances within the body. Recall that an action
potential in a muscle fiber is called a muscle action potential.
When an action
potential occurs in a neuron (nerve cell), it is called a nerve action
potential (nerve impulse).
The
production of graded potentials and action potentials depends on two basic
features of the plasma membrane of excitable cells: the existence of a resting
membrane potential and the presence of specific types of ion channels. Like most
other cells in the body, the plasma membrane of excitable cells exhibits a
membrane potential, an electrical potential difference (voltage) across the
membrane. In excitable cells, this voltage is termed the resting membrane
potential. The membrane potential is like voltage stored in a battery. If you
connect the positive and negative terminals of a battery with a piece of wire,
electrons will flow along the wire. This flow of charged particles is called
current. In living cells, the flow of ions (rather than electrons) constitutes
the electrical current.
Graded
potentials and action potentials occur because the membranes of neurons contain
many different kinds of ion channels that open or close in response to specific
stimuli. Because the lipid bilayer of the plasma membrane is a good electrical
insulator, the main paths for current to flow across the membrane are through
the ion channels.
Ion
Channels When ion channels are open, they allow specific ions to move across the
plasma membrane, down their electrochemical gradient—a concentration (chemical)
difference plus an electrical difference. Recall that ions move from areas of
higher concentration to areas of lower concentration (the chemical part of the
gradient). Also, positively charged cations move toward a negatively charged
area, and negatively charged anions move toward a positively charged area (the
electrical aspect of the gradient). As ions move, they create a flow of
electrical current that can change the membrane potential. Ion channels open
and close due to the presence of “gates.” The gate is a part of the channel
protein that can seal the channel pore shut or move aside to open the pore. The
electrical signals produced by neurons and muscle fibers rely on four types of
ion channels: leakage channels, ligand-gated channels, mechanically gated
channels, and voltage-gated channels.
1.
The gates of leakage channels randomly alternate between open and closed
positions. Typically, plasma membranes have many more potassium ion (K) leakage
channels than sodium ion (Na) leakage channels, and the potassium ion leakage
channels are leakier than the sodium ion leakage channels. Thus, the membrane’s
permeability to K is much higher than its permeability to Na.
2.
A ligand-gated channel opens and closes in response to a specific chemical
stimulus. A wide variety of chemical ligands— including neurotransmitters,
hormones, and particular ions—can open or close ligand-gated channels. The
neurotransmitter acetyl- choline, for example, opens cation channels that allow
Na and Ca2 to diffuse inward and K to diffuse outward
3.
A mechanically gated channel opens or closes in response to mechanical
stimulation in the form of vibration (such as sound waves), touch, pressure, or
tissue stretching. The force distorts the channel from its resting position,
opening the gate. Examples of mechanically gated channels are those found in
auditory receptors in the ears, in receptors that monitor stretching of internal
organs, and in touch receptors and pressure receptors in the skin.
4.
A voltage-gated channel opens in response to a change in membrane potential
(voltage). Voltage-gated channels participate in the generation and conduction
of action potentials.
Resting
Membrane Potential
The
resting membrane potential exists because of a small buildup of negative ions
in the cytosol along the inside of the membrane, and an equal buildup of
positive ions in the extra- cellular fluid along the outside surface of the
membrane. Such a separation of positive and negative electrical charges is a
form of potential energy, which is measured in mili volts (1 mV 0.001 V). The
greater the difference in charge across the membrane, the larger the membrane
potential (voltage). The buildup of charge occurs only very close to the
membrane. The cytosol or extracellular fluid elsewhere in the cell contains
equal numbers of positive and negative charges and is electrically neutral. The
resting membrane potential of a cell can be measured in the following way: The
tip of a recording microelectrode is inserted inside the cell, and a reference
electrode is placed outside the cell in the extracellular fluid. Electrodes are
devices that con- duct electrical charges. The recording microelectrode and the
reference electrode are connected to an instrument known as a voltmeter, which
detects the electrical difference (voltage) across the plasma membrane.
In neurons, the resting membrane potential ranges from 40 to 90 mV. A typical
value is 70 mV. The minus sign indicates that the inside of the cell is
negative relative to the outside. A cell that exhibits a membrane potential is
said to be polarized. Most body cells are polarized; the membrane potential
varies from 5 mV to 100 mV in different types of cells. The resting membrane
potential arises from three major factors: 1. Unequal distribution of ions in
the ECF and cytosol. A major factor that contributes to the resting membrane
potential is the unequal distribution of various ions in extracellular fluid and
cytosol. Extracellular fluid is rich in Na and chloride ions (Cl). In cytosol,
however, the main cation is K and the two dominant anions are phosphates
attached to molecules, such as the three phosphates in ATP, and amino acids in
proteins. Because the plasma membrane typically has more K leakage channels
than Na leakage channels, the number of potassium ions that diffuse down their
concentration gradient out of the cell into the ECF is greater than the number
of sodium ions that diffuse down their concentration gradient from the ECF into
the cell. As more and more positive potassium ions exit, the in- side of the
membrane becomes increasingly negative, and the outside of the membrane becomes
increasingly positive. 2. Inability of most anions to leave the cell. Another
factor contributes to the inside-negative resting membrane potential: Most
anions inside the cell are not free to leave. They cannot follow the K out of
the cell because they are attached to non-diffusible molecules such as ATP and
large proteins. 3. Electrogenic nature of the Na K ATPases. Membrane
permeability to Na is very low because there are only a few sodium leakage
channels. Nevertheless, sodium ions do slowly diffuse inward, down their
concentration gradient. Left unchecked, such inward leakage of Na would
eventually destroy the resting membrane potential. The small inward Na leak and
outward K leak are offset by the Na K ATPases (sodium–potassium pumps). These
pumps help maintain the resting membrane potential by pumping out Na as fast as
it leaks in. At the same time, the Na/K ATPases bring in K However, the
potassium ions eventually leak back out of the cell as they move down their
concentration gradient. Recall that the Na/K ATPases expel three Na for each
two K imported. Since these pumps remove more positive charges from the cell
than they bring into the cell, they are electrogenic, which means they
contribute to the negativity of the resting membrane potential. Their total
contribution, however, is very small: only 3 mV of the total 70 mV resting
membrane potential in a typical neuron.
Graded
Potentials
A
graded potential is a small deviation from the membrane potential that makes
the membrane either more polarized (inside more negative) or less polarized
(inside less negative). When the response makes the membrane more polarized
(inside more negative), it is termed a hyperpolarizing graded potential. When
the response makes the membrane less polarized (inside less negative), it is
termed a depolarizing graded potential. A graded potential occurs when a
stimulus causes mechanically gated or ligand-gated channels to open or close in
an excitable cell’s plasma membrane. Typically, mechanically gated channels and
ligand-gated channels can be present in the dendrites of sensory neurons, and
ligand-gated channels are numerous in the dendrites and cell bodies of inter
neurons and motor neurons. Hence, graded potentials occur mainly in the
dendrites and cell body of a neuron. To say that these electrical signals are
graded means that they vary in amplitude (size), depending on the strength of
the stimulus. They are larger or smaller depending on how many ligand-gated or
mechanically gated channels have opened (or closed) and how long each remains
open. The opening or closing of these ion channels alters the flow of specific
ions across the membrane, producing a flow of current that is localized, which
means that it spreads to adjacent regions along the plasma membrane in either
direction from the stimulus source for a short distance and then gradually dies
out as the charges are lost across the membrane through leakage channels.
This mode of travel by which graded potentials die out as they spread along the
membrane is known as decremental conduction. Because they die out within a few
millimeters of their point of origin, graded potentials are useful for
short-distance communication only. Although an individual graded potential
undergoes decremental conduction, it can become stronger and last longer by
sum- mating with other graded potentials. Summation is the process by which
graded potentials add together. If two depolarizing graded potentials
summate, the net result is a larger depolarizing graded potential. If two
hyperpolarizing graded potentials summate, the net result is a larger
hyperpolarizing graded potential. If two equal but opposite graded potentials
summate (one depolarizing and the other hyperpolarizing), then they cancel each
other out and the overall graded potential disappears. You will learn more
about the process of summation later in this chapter. Graded potentials have
different names depending on which type of stimulus causes them and where they
occur. For example, when a graded potential occurs in the dendrites or cell
body of a neuron in response to a neurotransmitter, it is called a post-
synaptic potential (explained shortly). On the other hand, the graded
potentials that occur in sensory receptors and sensory neurons are termed
receptor potentials and generator potentials.
Generation
of Action Potentials
An
action potential (AP) or impulse is a sequence of rapidly occurring events that
decrease and reverse the membrane potential and then eventually restore it to
the resting state. An action potential has two main phases: a
depolarizing phase and a repolarizing phase. During the depolarizing phase, the
negative membrane potential becomes less negative, reaches zero, and then
becomes positive. During the repolarizing phase, the membrane potential is
restored to the resting state of 70 mV. Following the repolarizing phase there
may be an after-hyperpolarizing phase, during which the membrane potential
temporarily becomes more negative than the resting level. Two types of
voltage-gated channels open and then close during an action potential.
These channels are present mainly in the axon plasma membrane and axon
terminals. The first channels that open, the voltage-gated Na channels, allow Na
to rush into the cell, which causes the depolarizing phase. Then voltage-gated
K channels open, allowing K to flow out, which produces the repolarizing phase.
The after-hyperpolarizing phase occurs when the voltage-gated K channels remain
open after the repolarizing phase ends. An action potential occurs in the
membrane of the axon of a neuron when depolarization reaches a certain level
termed the threshold (about 55 mV in many neurons). Different neurons may have
different thresholds for generation of an action potential, but the threshold
in a particular neuron usually is constant. The generation of an action
potential depends on whether a particular stimulus is able to bring the
membrane potential to threshold. An action potential will not occur in response
to a sub- threshold stimulus, a stimulus that is a weak depolarization that
cannot bring the membrane potential to threshold. However, an action potential
will occur in response to a threshold stimulus, a stimulus that is just strong
enough to de- polarize the membrane to threshold. Several action potentials
will form in response to a supra threshold stimulus, a stimulus that is strong
enough to depolarize the membrane above threshold. Each of the action
potentials caused by a supra threshold stimulus has the same amplitude (size)
as an action potential caused by a threshold stimulus. Therefore, once an
action potential is generated, the amplitude of an action potential is always
the same and does not depend on stimulus intensity. Instead, the greater the
stimulus strength above threshold, the greater the frequency of the action
potentials until a maximum frequency is reached as determined by the absolute
refractory period (described shortly). As you have just learned, an action
potential is generated in response to a threshold stimulus, but does not form
when there is a sub threshold stimulus. In other words, an action potential
either occurs completely or it does not occur at all. This characteristic of an
action potential is known as the all-or-none principle. The all-or-none
principle of the action potential is similar to pushing the first domino in a
long row of standing dominoes. When the push on the first domino is strong
enough (when depolarization reaches threshold), that domino falls against the
second domino, and the entire row topples (an action potential occurs).
Stronger pushes on the first domino produce the identical effect—toppling of the
entire row. Thus, pushing on the first domino produces an all-or-none event: The
dominoes all fall or none fall.
Depolarizing
Phase: When a depolarizing graded potential or some other stimulus causes the
membrane of the axon to depolarize to threshold, voltage-gated Na channels open
rapidly. Both the electrical and the chemical gradients favor inward movement
of Na and the resulting in rush of Na causes the depolarizing phase of the
action potential. The inflow of Na changes the membrane potential from 55 mV to
30 mV. At the peak of the action potential, the inside of the membrane is 30 mV
more positive than the outside. Each voltage-gated Na channel has two separate
gates, an activation gate and an inactivation gate. In the resting state of a
voltage-gated Na channel, the inactivation gate is open, but the activation
gate is closed. As a result, Na cannot move into the cell through these
channels. At thresh- old, voltage-gated Na channels are activated. In the
activated state of a voltage-gated Na channel, both the activation and in-
activation gates in the channel are open and Na inflow begins. As more channels
open, Na inflow in- creases, the membrane depolarizes further, and more Na
channels open. This is an example of a positive feedback mechanism. During the
few ten-thousandths of a second that the voltage- gated Na channel is open,
about 20,000 Na flow across the membrane and change the membrane potential
considerably. But the concentration of Na hardly changes because of the
millions of Na present in the extracellular fluid. The sodium–potassium pumps
easily bail out the 20,000 or so Na that enter the cell during a single action
potential and maintain the low concentration of Na inside the cell.
Repolarizing
Phase: Shortly after the activation gates of the voltage-gated Na channels
open, the inactivation gates close. Now the voltage-gated Na channel is in an
inactivated state. In addition to opening voltage-gated Na channels, a
threshold- level depolarization also opens voltage-gated K channels. Because
the voltage-gated K channels open more slowly, their opening occurs at about
the same time the voltage-gated Na channels are closing. The slower opening of
voltage-gated K channels and the closing of previously open voltage-gated Na
channels produce the repolarizing phase of the action potential. As the Na
channels are inactivated, Na inflow slows. At the same time, the K channels are
opening, accelerating K outflow. Slowing of Na inflow and acceleration of K
outflow causes the membrane potential to change from 30 mV to 70 mV.
Repolarization also allows inactivated Na channels to revert to the resting
state.
After-hyperpolarizing
Phase While the voltage-gated K channels are open, outflow of K may be large
enough to cause an after-hyperpolarizing phase of the action potential. During
this phase, the voltage-gated K channels remain open and the membrane potential
becomes even more negative (about 90 mV). As the voltage-gated K channels
close, the membrane potential returns to the resting level of 70 mV. Unlike
voltage-gated Na channels, most voltage-gated K channels do not exhibit an
inactivated state. Instead, they alternate between closed (resting) and open
(activated) states.
Refractory
Period: The period of time after an action potential begins during which an
excitable cell cannot generate another action potential in response to a normal
threshold stimulus is called the refractory period. During the absolute
refractory period, even a very strong stimulus cannot initiate a second action
potential. This period coincides with the period of Na channel activation and
inactivation. Inactivated Na channels cannot reopen; they first must return to
the resting state. In contrast to action potentials, graded potentials do not
exhibit a refractory period. Large-diameter axons have a larger surface area
and have a brief absolute refractory period of about 0.4 msec. Because a second
nerve impulse can arise very quickly, up to 1000 impulses per second are
possible. Small-diameter axons have absolute refractory periods as long as 4
msec, enabling them to transmit a maximum of 250 impulses per second. Under
normal body conditions, the maximum frequency of nerve impulses in different
axons ranges between 10 and 1000 per second. The relative refractory period is
the period of time during which a second action potential can be initiated, but
only by a larger-than-normal stimulus. It coincides with the period when the
voltage-gated K channels are still open after inactivated Na channels have
returned to their resting state.
SIGNAL
TRANSMISSION AT SYNAPSES
Synapses
are essential for homeostasis because they allow information to be filtered and
integrated. During learning, the structure and function of particular synapses
change. The changes may allow some signals to be transmitted while others are
blocked. For example, the changes in your synapses from studying will determine
how well you do on your anatomy and physiology tests! Synapses are also
important because some diseases and neurological disorders result from disruptions
of synaptic communication, and many therapeutic and addictive chemicals affect
the body at these junctions. At a synapse between neurons, the neuron sending
the signal is called the presynaptic neuron, and the neuron receiving the
message is called the postsynaptic neuron. Most synapses are either
axodendritic (from axon to dendrite), axosomatic (from axon to cell body), or
axoaxonic (from axon to axon). The two types of synapses—electrical and
chemical—differ both structurally and functionally.
Electrical
Synapses: At an electrical synapse, action potentials (impulses) conduct
directly between adjacent cells through structures called gap junctions. Each
gap junction contains a hundred or so tubular connexons, which act like tunnels
to connect the cytosol of the two cells directly. As ions flow from one cell to
the next through the connexons, the action potential spreads from cell to cell.
Gap junctions are common in visceral smooth muscle, cardiac muscle, and the
developing embryo. They also occur in the CNS. Electrical synapses have two
main advantages: 1. faster communication. Because action potentials conduct
directly through gap junctions, electrical synapses are faster than chemical
synapses. At an electrical synapse, the action potential passes directly from
the presynaptic cell to the postsynaptic cell. The events that occur at a
chemical synapse take some time and delay communication slightly. 2.
Synchronization. Electrical synapses can synchronize (coordinate) the activity
of a group of neurons or muscle fibers. In other words, a large number of
neurons or muscle fibers can produce action potentials in unison if they are
connected by gap junctions. The value of synchronized action potentials in the
heart or in visceral smooth muscle is coordinated contraction of these fibers to
produce a heartbeat or move food through the gastrointestinal tract.
Chemical
Synapses: Although the plasma membranes of presynaptic and postsynaptic neurons
in a chemical synapse are close, they do not touch. They are separated by the
synaptic cleft, a space of 20–50 nm* that is filled with interstitial fluid.
Nerve impulses cannot conduct across the synaptic cleft, so an alternative,
indirect form of communication occurs. In response to a nerve impulse, the
presynaptic neuron releases a neurotransmitter that diffuses through the fluid
in the synaptic cleft and binds to receptors in the plasma membrane of the
postsynaptic neuron. The postsynaptic neuron receives the chemical signal and
in turn produces a postsynaptic potential, a type of graded potential. Thus,
the presynaptic neuron converts an electrical signal (nerve impulse) into a
chemical signal (released neurotransmitter). The postsynaptic neuron receives
the chemical signal and in turn generates an electrical signal (postsynaptic
potential). The time required for these processes at a chemical synapse, a
synaptic delay of about 0.5 msec, is the reason that chemical synapses relay
signals more slowly than electrical synapses. A typical chemical synapse
transmits a signal as follows:
●
A nerve impulse arrives at a synaptic end bulb (or at a varicosity) of a
presynaptic axon.
●
The depolarizing phase of the nerve impulse opens voltage- gated Ca2 channels,
which are present in the membrane of synaptic end bulbs. Because calcium ions
are more concentrated in the extracellular fluid, Ca2 flows inward through the
opened channels.
●
An increase in the concentration of Ca2 inside the presynaptic neuron serves as
a signal that triggers exocytosis of the synaptic vesicles. As vesicle
membranes merge with the plasma membrane, neurotransmitter molecules within the
vesicles are released into the synaptic cleft. Each synaptic vesicle contains
several thousand molecules of neurotransmitter.
●
The neurotransmitter molecules diffuse across the synaptic cleft and bind to
neurotransmitter receptors in the postsynaptic neuron’s plasma membrane. Not
all neurotransmitters bind to ionotropic receptors; some bind to metabotropic
receptors (described shortly).
●
Binding of neurotransmitter molecules to their receptors on ligand-gated
channels opens the channels and allows particular ions to flow across the
membrane.
●
As ions flow through the opened channels, the voltage across the membrane changes.
This change in membrane voltage is a postsynaptic potential. Depending on which
ions the channels admit, the postsynaptic potential may be a depolarization or
a hyperpolarization. For example, opening of Na channels allows inflow of Na
which causes de- polarization. However, opening of Cl or K channels causes
hyperpolarization. Opening Cl channels permits Cl to move into the cell, while
opening the K channels allows K to move out—in either event, the inside of the
cell becomes more negative.
●
When a depolarizing postsynaptic potential reaches threshold, it triggers an
action potential in the axon of the post- synaptic neuron. At most chemical
synapses, only one-way information transfer can occur—from a presynaptic neuron
to a postsynaptic neuron or an effector, such as a muscle fiber or a gland cell.
For ex- ample, synaptic transmission at a neuromuscular junction (NMJ) proceeds
from a somatic motor neuron to a skeletal muscle fiber (but not in the opposite
direction). Only synaptic end bulbs of presynaptic neurons can release
neurotransmitter, and only the postsynaptic neuron’s membrane has the receptor
proteins that can recognize and bind that neurotransmitter. As a result, action
potentials move in one direction.
Excitatory
and Inhibitory Postsynaptic Potentials:
A neurotransmitter causes either
an excitatory or an inhibitory graded potential. A neurotransmitter that
depolarizes the postsynaptic membrane is excitatory because it brings the
membrane closer to threshold. A depolarizing postsynaptic potential is called
an excitatory postsynaptic potential (EPSP). Although a single EPSP normally
does not initiate a nerve impulse, the postsynaptic cell does become more
excitable. Because it is partially depolarized, it is more likely to reach
threshold when the next EPSP occurs. A neurotransmitter that causes
hyperpolarization of the post- synaptic membrane is inhibitory. During
hyperpolarization, generation of an action potential is more difficult than
usual because the membrane potential becomes inside more negative and thus even
farther from threshold than in its resting state. A hyperpolarizing
postsynaptic potential is termed an inhibitory postsynaptic potential (IPSP).
Neurotransmitters
About
100 substances are either known or suspected neurotransmitters. Some
neurotransmitters bind to their receptors and act quickly to open or close ion
channels in the membrane. Others act more slowly via second-messenger systems
to influence chemical reactions inside cells. The result of either process can
be excitation or inhibition of postsynaptic neurons. Many neurotransmitters are
also hormones released into the bloodstream by endocrine cells in organs
throughout the body. Within the brain, certain neurons, called neurosecretory
cells, also secrete hormones. Neurotransmitters can be divided into two classes
based on size: small-molecule neurotransmitters and neuropeptides.
Small-Molecule
Neurotransmitters
The
small-molecule neurotransmitters include acetylcholine, amino acids, biogenic
amines, ATP and other purines, and nitric oxide.
Acetylcholine
The best-studied neurotransmitter is acetylcholine (ACh), which is released by
many PNS neurons and by some CNS neurons. ACh is an excitatory neurotransmitter
at some synapses, such as the neuromuscular junction, where the binding of ACh
to ionotropic receptors opens cation channels. It is also an inhibitory
neurotransmitter at other synapses, where it binds to metabotropic receptors
coupled to G proteins that open K channels. For example, ACh slows heart rate
at inhibitory synapses made by parasympathetic neurons of the vagus (X) nerve.
The enzyme acetylcholinesterase (AChE) inactivates ACh by splitting it into
acetate and choline fragments.
Amino
Acids: Several amino acids are neurotransmitters in the CNS. Glutamate
(glutamic acid) and aspartate (aspartic acid) have powerful excitatory effects.
Most excitatory neurons in the CNS and perhaps half of the synapses in the
brain communicate via glutamate. At some glutamate synapses, binding of the
neuro- transmitter to ionotropic receptors opens cation channels. The
consequent inflow of cations (mainly Na ions) produces an EPSP. Inactivation of
glutamate occurs via reuptake. Glutamate transporters actively transport
glutamate back into the synaptic end bulbs and neighboring neuroglia. Gamma
amino butyric acid (GABA) and glycine are important inhibitory
neurotransmitters. At many synapses, the binding of GABA to ionotropic
receptors opens Cl channels. GABA is found only in the CNS, where it is the
most common inhibitory neurotransmitter. As many as one-third of all brain
synapses use GABA. Antianxiety drugs such as diazepam enhance the action of
GABA. Like GABA, the binding of glycine to ionotropic receptors opens Cl
channels. About half of the inhibitory synapses in the spinal cord use
the amino acid glycine; the rest use GABA.
Biogenic
Amines: Certain amino acids are modified and decarboxylated (carboxyl group
removed) to produce biogenic amines. Those that are prevalent in the nervous
system include norepinephrine, epinephrine, dopamine, and serotonin. Most
biogenic amines bind to metabotropic receptors; there are many different types
of metabotropic receptors for each biogenic amine. Biogenic amines may cause
either excitation or inhibition, depending on the type of metabotropic receptor
at the synapse. Norepinephrine (NE) plays roles in arousal (awakening from deep
sleep), dreaming, and regulating mood. A smaller number of neurons in the brain
use epinephrine as a neurotransmitter. Both epinephrine and norepinephrine also
serve as hormones. Cells of the adrenal medulla, the inner portion of the
adrenal gland, release them into the blood. Brain neurons containing the
neurotransmitter dopamine (DA) are active during emotional responses, addictive
behaviors, and pleasurable experiences. In addition, dopamine-releasing neurons
help regulate skeletal muscle tone and some aspects of movement due to
contraction of skeletal muscles. The muscular stiffness that occurs in
Parkinson disease is due to degeneration of neurons that release dopamine. One
form of schizophrenia is due to accumulation of excess dopamine.
Norepinephrine, dopamine, and epinephrine are classified chemically as
catecholamines. They all include an amino group (-NH2) and a catechol ring
composed of six carbons and two adjacent hydroxyl (-OH) groups. Catecholamines
are synthesized from the amino acid tyrosine. Inactivation of catecholamines
occurs via reuptake into synaptic end bulbs. Then they are either recycled back
into the synaptic vesicles or destroyed by the enzymes. The two enzymes that
break down catecholamines are catechol-O-methyltransferase or COMT, and
monoamine oxidase or MAO. Serotonin, also known as 5-hydroxytryptamine (5-HT),
is concentrated in the neurons in a part of the brain called the raphe nucleus.
It is thought to be involved in sensory perception, temperature regulation,
control of mood, appetite, and the induction of sleep
ATP
and Other Purines: The characteristic ring structure of the adenosine portion
of ATP is called a purine ring. Adenosine itself, as well as its triphosphate,
diphosphate, and monophosphate derivatives (ATP, ADP, and AMP), is an
excitatory neurotransmitter in both the CNS and the PNS. Most of the synaptic
vesicles that contain ATP also contain another neurotransmitter. In the PNS,
ATP and norepinephrine are released together from some sympathetic neurons;
some parasympathetic neurons release ATP and acetylcholine in the same
vesicles.
Nitric
Oxide: The simple gas nitric oxide (NO) is an important neurotransmitter that
has widespread effects throughout the body. NO contains a single nitrogen atom,
in contrast to nitrous oxide (N2O), or laughing gas, which has two nitrogen
atoms. N2O is sometimes used as an anesthetic during dental procedures. The
enzyme nitric oxide synthase (NOS) catalyzes formation of NO from the amino
acid arginine. Based on the presence of NOS, it is estimated that more than 2%
of the neurons in the brain produce NO. Unlike all previously known
neurotransmitters, NO is not synthesized in advance and packaged into synaptic
vesicles. Rather, it is formed on demand and acts immediately. Its action is
brief because NO is a highly reactive free radical. It exists for less than 10
seconds before it combines with oxygen and water to form inactive nitrates and
nitrites. Because NO is lipid-soluble, it diffuses from cells that produce it
into neighboring cells, where it activates an enzyme for production of a second
messenger called cyclic GMP. Some research suggests that NO plays a role in
memory and learning. The first recognition of NO as a regulatory molecule was
the discovery in 1987 that a chemical called EDRF (endothelium- derived
relaxing factor) was actually NO. Endothelial cells in blood vessel walls
release NO, which diffuses into neighboring smooth muscle cells and causes
relaxation. The result is vasodilation, an increase in blood vessel diameter.
The effects of such vasodilation range from a lowering of blood pressure to
erection of the penis in males. Sildenafil alleviates erectile dysfunction
(impotence) by enhancing the effect of NO. In larger quantities, NO is highly
toxic. Phagocytic cells, such as macrophages and certain white blood cells,
produce NO to kill microbes and tumor cells.
Neuropeptides:
Neurotransmitters consisting of 3 to 40 amino acids linked by peptide bonds
called neuropeptides are numerous and widespread in both the CNS and the
PNS. Neuropeptides bind to metabotropic receptors and have excitatory or
inhibitory actions, depending on the type of metabotropic receptor at the
synapse. Neuropeptides are formed in the neuron cell body, packaged into
vesicles, and transported to axon terminals. Besides their role as
neurotransmitters, many neuropeptides serve as hormones that regulate
physiological responses elsewhere in the body. Scientists discovered that certain
brain neurons have plasma membrane receptors for opiate drugs such as morphine
and heroin. The quest to find the naturally occurring substances that use these
receptors brought to light the first neuropeptides: two molecules, each a chain
of five amino acids, named enkephalins. Their potent analgesic (pain-relieving)
effect is 200 times stronger than morphine. Other so called opioid pep- tides
include the endorphins and dynorphins. It is thought that opioid peptides are
the body’s natural painkillers. Acupuncture may produce analgesia (loss of pain
sensation) by increasing the release of opioids. These neuropeptides have also
been linked to improved memory and learning; feelings of pleasure or euphoria;
control of body temperature; regulation of hormones that affect the onset of
puberty, sexual drive, and reproduction; and mental illnesses such as
depression and schizophrenia. Another neuropeptide, substance P, is released by
neurons that transmit pain-related input from peripheral pain receptors into the
central nervous system, enhancing the perception of pain. Enkephalin and
endorphin suppress the release of sub- stance P, thus decreasing the number of
nerve impulses being relayed to the brain for pain sensations. Substance P has
also been shown to counter the effects of certain nerve-damaging chemicals,
prompting speculation that it might prove useful as a treatment for nerve
degeneration.
Structure
of Neurotransmitter Receptors
As
you have already learned, neurotransmitters released from a presynaptic neuron
bind to neurotransmitter receptors in the plasma membrane of a postsynaptic
cell. Each type of neuro- transmitter receptor has one or more neurotransmitter
binding sites where its specific neurotransmitter binds. When a neuro-
transmitter binds to the correct neurotransmitter receptor, an ion channel
opens and a postsynaptic potential (either an EPSP or IPSP) forms in the
membrane of the postsynaptic cell. Neuro- transmitter receptors are classified
as either ionotropic receptors or metabotropic receptors based on whether the
neurotransmitter binding site and the ion channel are components of the same
protein or are components of different proteins.
Ionotropic
Receptors: An ionotropic receptor is a type of neurotransmitter receptor that
contains a neurotransmitter binding site and an ion channel. In other words,
the neurotransmitter binding site and the ion channel are components of the
same protein. An ionotropic receptor is a type of ligand-gated
channel. In the absence of neurotransmitter (the ligand), the ion channel
component of the ionotropic receptor is closed. When the correct
neurotransmitter binds to the ionotropic receptor, the ion channel opens, and
an EPSP or IPSP occurs in the postsynaptic cell. Many excitatory
neurotransmitters bind to ionotropic receptors that contain cation channels.
EPSPs result from opening these cation channels. When cation channels
open, they allow passage of the three most plentiful cations (Na K and Ca2
through the postsynaptic cell membrane, but Na inflow is greater than either Ca2
inflow or K outflow and the inside of the postsynaptic cell becomes less negative
(de- polarized). Many inhibitory neurotransmitters bind to ionotropic receptors
that contain chloride channels. IPSPs result from opening these Cl channels. When
Cl channels open, a larger number of chloride ions diffuse inward. The inward
flow of Cl ions causes the inside of the postsynaptic cell to become more
negative (hyperpolarized).
Metabotropic
Receptors: A metabotropic receptor is a type of neurotransmitter receptor that
contains a neurotransmitter binding site, but lacks an ion channel as part of
its structure. However, a metabotropic receptor is coupled to a separate ion
channel by a type of membrane protein called a G protein. When a
neurotransmitter binds to a metabotropic receptor, the G protein either
directly opens (or closes) the ion channel or it may act indirectly by
activating an- other molecule, a “second messenger,” in the cytosol, which in
turn opens (or closes) the ion channel (see Chapter 18 for a detailed
discussion of G proteins). Thus, a metabotropic receptor differs from an
ionotropic receptor in that the neurotransmitter binding site and the ion
channel are components of different proteins. Some inhibitory neurotransmitters
bind to metabotropic receptors that are linked to K channels IPSPs result from
the opening of these K channels. When K channels open, a larger number of
potassium ions diffuses outward. The outward flow of K ions causes the inside of
the postsynaptic cell to become more negative (hyperpolarized).
Different
Postsynaptic Effects for the Same Neurotransmitter The same neurotransmitter
can be excitatory at some synapses and inhibitory at other synapses, depending
on the structure of the neurotransmitter receptor to which it binds. For
example, at some excitatory synapses acetylcholine (ACh) binds to ionotropic
receptors that contains cation channels that open and subsequently generate
EPSPs in the postsynaptic cell. By contrast, at some inhibitory synapses ACh
binds to metabotropic receptors coupled to G proteins that open K channels,
resulting in the formation of IPSPs in the postsynaptic cell.
Removal
of Neurotransmitter
Removal
of the neurotransmitter from the synaptic cleft is essential for normal
synaptic function. If a neurotransmitter could linger in the synaptic cleft, it
would influence the postsynaptic neuron, muscle fiber, or gland cell indefinitely.
Neurotransmitter is removed in three ways: 1. Diffusion. Some of the released
neurotransmitter molecules diffuse away from the synaptic cleft. Once a
neurotransmitter molecule is out of reach of its receptors, it can no longer
exert an effect. 2. Enzymatic degradation. Certain neurotransmitters are
inactivated through enzymatic degradation. For example, the enzyme
acetylcholinesterase breaks down acetylcholine in the synaptic cleft. 3. Uptake
by cells. Many neurotransmitters are actively trans- ported back into the
neuron that released them (reuptake). Others are transported into neighboring
neuroglia (uptake). The neurons that release norepinephrine, for example,
rapidly take up the norepinephrine and recycle it into new synaptic vesicles.
The membrane proteins that accomplish such uptake are called neurotransmitter
transporters.
Spatial
and Temporal Summation of Postsynaptic Potentials
A
typical neuron in the CNS receives input from 1000 to 10,000 synapses.
Integration of these inputs involves summation of the postsynaptic potentials
that form in the postsynaptic neuron. Recall that summation is the process by
which graded potentials add together. The greater the summation of EPSPs, the
greater the chance that threshold will be reached. At threshold, one or more
nerve impulses (action potentials) arise. There are two types of summation: spatial
summation and temporal summation. Spatial summation is summation of
postsynaptic potentials in response to stimuli that occur at different
locations in the membrane of a postsynaptic cell at the same time. For example,
spatial summation results from the buildup of neurotransmitter released
simultaneously by several presynaptic end bulbs. Temporal summation is
summation of postsynaptic potentials in response to stimuli that occur at the
same location in the membrane of the postsynaptic cell but at different times.
For example, temporal summation results from buildup of neurotransmitter
released by a single presynaptic end bulb two or more times in rapid
succession. Because a typical EPSP lasts about 15msec, the second (and
subsequent) release of neurotransmitter must occur soon after the first one if
temporal summation is to occur. Summation is rather like a vote on the
Internet. Many people voting “yes” or “no” on an issue at the same time can be
compared to spatial summation. One person voting repeatedly and rapidly is like
temporal summation. Most of the time, spatial and temporal summations are
acting together to influence the chance that a neuron fires an action potential.
A
single postsynaptic neuron receives input from many pre- synaptic neurons, some
of which release excitatory neurotransmitters and some of which release
inhibitory neurotransmitters. The sum of all the excitatory and inhibitory
effects at any given time determines the effect on the postsynaptic neuron,
which may respond in the following ways: 1. EPSP. If the total excitatory
effects are greater than the total inhibitory effects but less than the
threshold level of stimulation, the result is an EPSP that does not reach
threshold. Following an EPSP, subsequent stimuli can more easily generate a
nerve impulse through summation because the neuron is partially depolarized. 2.
Nerve impulse(s). If the total excitatory effects are greater than the total
inhibitory effects and threshold is reached, one or more nerve impulses (action
potentials) will be triggered. Impulses continue to be generated as long as the
EPSP is at or above the threshold level. 3. IPSP. If the total inhibitory
effects are greater than the excitatory effects, the membrane hyperpolarizes
(IPSP). The result is inhibition of the postsynaptic neuron and an inability to
generate a nerve impulse.
RELATED PICTURES:
 |
| STRUCTURE OF NEURON |
 |
| TYPES OF NEURON |
 |
| ION CHANNELS TO GENERATE ACTION POTENTIAL |
 |
| PROPAGATION OF ACTION POTENTIAL |
 |
| DIFFERENT NEURO PEPTIDES & THEIR FUNCTION |
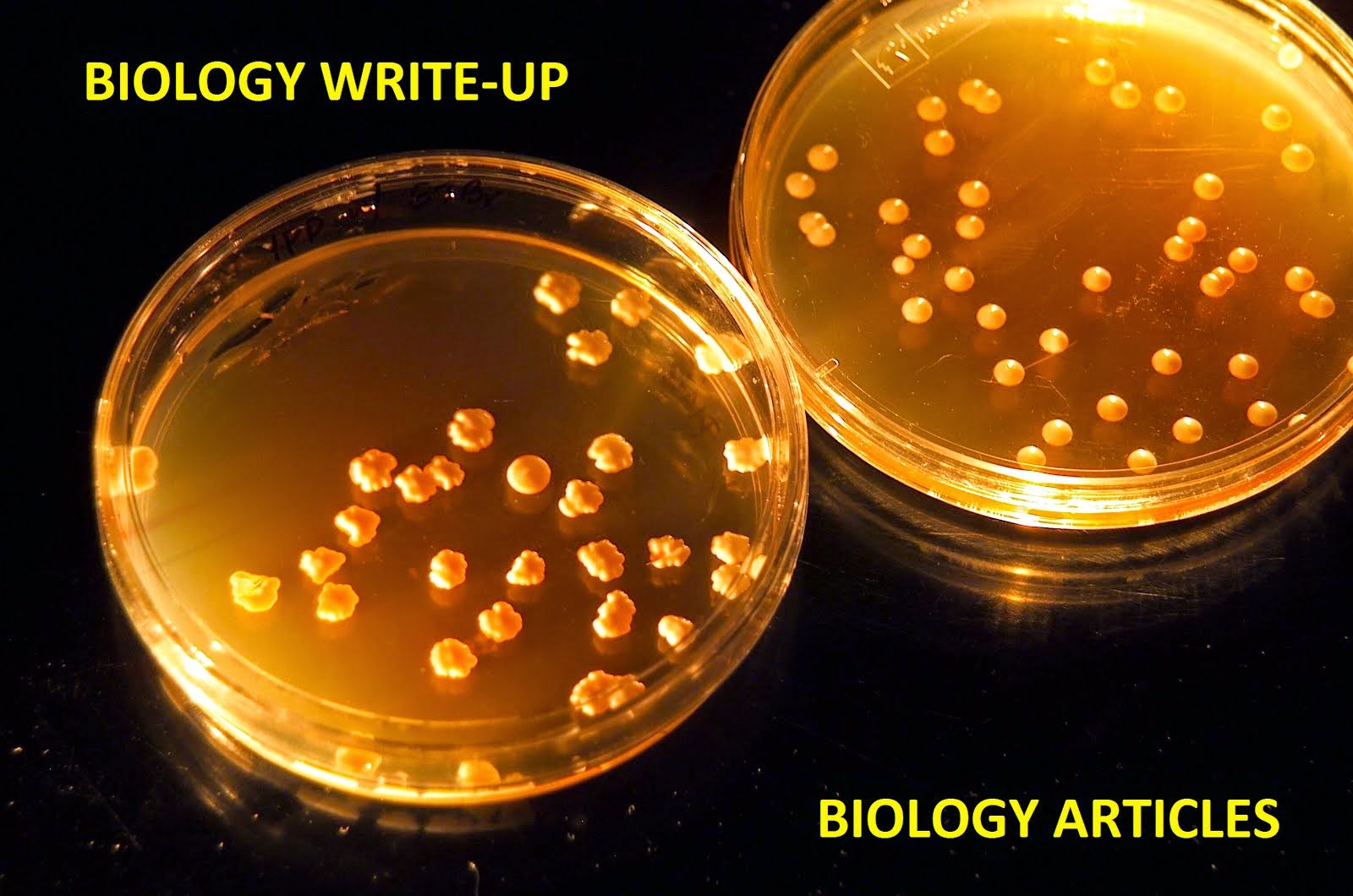
No comments:
Post a Comment